From Discovery to Clinic: A Comprehensive Guide to Clinically Validating Novel Enzyme Biomarkers
This article provides a systematic roadmap for researchers and drug development professionals navigating the complex process of clinically validating novel enzyme biomarkers.
From Discovery to Clinic: A Comprehensive Guide to Clinically Validating Novel Enzyme Biomarkers
Abstract
This article provides a systematic roadmap for researchers and drug development professionals navigating the complex process of clinically validating novel enzyme biomarkers. It covers the journey from foundational discovery and biological rationale to advanced methodological applications, tackling common troubleshooting challenges, and navigating the evolving regulatory landscape for qualification. By synthesizing current best practices, technological advancements, and statistical considerations, this guide aims to bridge the gap between promising experimental findings and the robust clinical evidence required for biomarker integration into diagnostic and therapeutic development, ultimately accelerating the path to personalized medicine.
Laying the Groundwork: Defining Novel Enzyme Biomarkers and Their Clinical Potential
What Makes an Enzyme a 'Novel' Biomarker? Definition and Key Characteristics
In the rapidly evolving field of clinical diagnostics and therapeutic development, a novel enzyme biomarker is defined as a recently discovered or applied enzymatic molecule that provides a specific, measurable indicator of biological processes, pathogenic states, or pharmacological responses to therapeutic intervention. The "novel" designation encompasses not only newly discovered enzymes but also established enzymes being applied to new clinical contexts, offering enhanced diagnostic or prognostic capabilities compared to existing biomarkers. These biomarkers are characterized by improved specificity, sensitivity, and clinical utility for early disease detection, accurate prognosis, and precise monitoring of therapeutic responses, particularly in areas of unmet medical need where traditional biomarkers demonstrate limitations [1] [2].
The validation pathway for novel enzyme biomarkers requires rigorous analytical validation, clinical qualification, and context-specific utilization to meet regulatory standards and achieve clinical adoption. The emergence of novel enzymes as biomarkers is being driven by advancements in 'omics' technologies, multiplexed assay platforms, and a growing understanding of enzymatic roles in disease pathophysiology, positioning them as critical tools in the advancement of precision medicine [1] [3] [4].
Enzymes have served as fundamental biomarkers in clinical chemistry for decades, with historically established examples including alanine aminotransferase (ALT) for liver function, creatine kinase-MB (CK-MB) for cardiac damage, and amylase for pancreatitis [2] [5]. However, significant limitations in these conventional biomarkers—including lack of tissue specificity, suboptimal sensitivity for early detection, and interference from non-pathological conditions—have driven the search for novel enzymatic indicators with enhanced performance characteristics [2] [6].
The definition of "novel" in this context extends beyond mere discovery chronology to encompass several key dimensions:
- Application Novelty: Known enzymes applied to new disease indications or clinical contexts
- Methodological Novelty: Enzymes measurable through new technological platforms with superior performance
- Informational Novelty: Enzymes that provide fundamentally new insights into disease mechanisms or treatment responses
- Regulatory Novelty: Enzymes that have recently received regulatory qualification for specific contexts of use [2] [6]
This evolution reflects a paradigm shift from traditional, single-marker approaches toward multiplexed, context-specific biomarker strategies that offer greater precision in clinical decision-making and therapeutic development [1] [7].
Defining Characteristics of Novel Enzyme Biomarkers
Enhanced Specificity and Sensitivity
Novel enzyme biomarkers demonstrate significantly improved tissue and pathway specificity compared to traditional markers, enabling more accurate differentiation between disease states and reducing false positives. For example, glutamate dehydrogenase (GLDH) has recently been qualified by the FDA as a specific biomarker for drug-induced liver injury in patients with muscle disease, where traditional markers like ALT and AST are confounded by concurrent muscle damage [6]. This enhanced specificity directly addresses a long-standing challenge in safety monitoring for clinical trials involving patients with neuromuscular disorders.
Clinical Utility in Early Detection and Monitoring
A defining characteristic of novel enzyme biomarkers is their ability to facilitate earlier disease detection and more precise therapy monitoring than established alternatives. Thymidine kinase 1 (TK1), for instance, has emerged as a sensitive serum biomarker for early diagnosis, prognosis, and therapy monitoring in breast cancer, often detecting disease recurrence or treatment response before clinical manifestations become apparent [2]. Similarly, glycogen phosphorylase BB (GPBB) demonstrates superior performance in detecting myocardial infarction within 4 hours of symptom onset, providing a critical diagnostic window for intervention [5].
Mechanistic Link to Disease Pathways
Unlike traditional biomarkers that may represent general indicators of tissue damage, novel enzyme biomarkers often have a direct pathophysiological connection to specific disease mechanisms. Enzymes such as cathepsins (B, D, and L) are not merely leakage markers but actively participate in tumor angiogenesis and proliferation processes in ovarian, pancreatic, colorectal, breast, and lung cancers [5]. This mechanistic relationship enhances their biological plausibility and strengthens their correlation with disease progression and therapeutic response.
Qualification Through Rigorous Validation Frameworks
Novel enzyme biomarkers undergo systematic validation through established regulatory frameworks such as the FDA-NIH Biomarkers, EndpointS, and other Tools (BEST) resource, which defines specific biomarker categories including diagnostic, monitoring, pharmacodynamic/response, predictive, prognostic, safety, and susceptibility/risk biomarkers [1]. The successful qualification of GLDH through the FDA's Biomarker Qualification Program exemplifies the rigorous evidentiary standards required for novel biomarker adoption in clinical trials and practice [6].
Classification and Regulatory Context
Biomarker Categories and Definitions
The BEST resource establishes precise definitions for biomarker categories that are essential for understanding the application of novel enzymes:
| Biomarker Category | Definition | Example Novel Enzymes |
|---|---|---|
| Diagnostic Biomarker | Detects or confirms presence of a disease or identifies individuals with a disease subtype | Carbonic anhydrase XII (pleural fluid for lung cancer) [2] |
| Monitoring Biomarker | Measured serially to assess disease status or evidence of exposure/effect | Thioredoxin reductase (plasma/serum for liver cancer therapy monitoring) [2] |
| Prognostic Biomarker | Predicts disease recurrence, progression, or other clinical outcomes | Caspase-3/7 (serum for head and neck squamous cell carcinoma) [2] |
| Predictive Biomarker | Identifies individuals more likely to respond to a specific therapeutic | Separase (peripheral blood for chronic myeloid leukemia) [2] |
| Safety Biomarker | Measured to indicate likelihood of adverse events | GLDH (serum for drug-induced liver injury) [6] |
| Pharmacodynamic/Response Biomarker | Shows biological response to therapeutic intervention | Ecto-5'-nucleotidase (plasma for breast cancer treatment response) [2] |
Regulatory Validation Pathway
The pathway from discovery to clinical implementation for novel enzyme biomarkers involves multiple validation stages:
Biomarker Validation Pathway
This validation pathway requires extensive evidence generation, with approximately 77% of biomarker qualification challenges linked to assay validity issues, highlighting the critical importance of methodological rigor [8].
Comparative Analysis: Novel vs. Traditional Enzyme Biomarkers
Performance Characteristics Comparison
| Characteristic | Traditional Enzyme Biomarkers | Novel Enzyme Biomarkers | Clinical Implications |
|---|---|---|---|
| Specificity | Often limited tissue specificity (e.g., ALT elevated in both liver and muscle damage) [6] | Enhanced tissue specificity (e.g., GLDH primarily hepatic) [6] | Reduced false positives, accurate differential diagnosis |
| Sensitivity | Moderate sensitivity for established disease | Higher sensitivity for early-stage detection (e.g., TK1 in breast cancer) [2] | Earlier intervention, improved outcomes |
| Mechanistic Link | Frequently correlates with tissue damage without direct disease mechanism involvement | Direct involvement in disease pathways (e.g., cathepsins in tumor angiogenesis) [5] | Better correlation with disease progression, superior therapeutic monitoring |
| Dynamic Range | Often limited analytical range | Broader dynamic range enabled by advanced detection platforms [8] | Accurate quantification across disease stages |
| Multiplexing Capability | Typically measured individually | Compatible with multiplexed panels (e.g., U-PLEX platform) [8] | Comprehensive biomarker signatures, improved diagnostic accuracy |
Clinical Application Comparison
| Disease Area | Traditional Enzyme Biomarkers | Novel Enzyme Biomarkers | Advancement Represented |
|---|---|---|---|
| Liver Safety Monitoring | ALT, AST (confounded by muscle disease) [6] | GLDH (liver-specific) [6] | Specific biomarker for patients with comorbid muscle conditions |
| Cancer Diagnostics | PSA, CA-125 (limited specificity) | TK1, cathepsins, carbonic anhydrase XII [2] [5] | Earlier detection, molecular subtyping, therapy monitoring |
| Cardiac Injury | CK-MB, myoglobin | GPBB (detectable within 4 hours) [5] | Earlier diagnosis of myocardial infarction |
| Bone Disorders | ALP (limited specificity) | TRAP (specific to osteoclast activity) [5] | Distinction between different bone pathologies |
Experimental Protocols for Validation
Analytical Validation Framework
Robust analytical validation is fundamental to establishing novel enzyme biomarkers. Key methodological approaches include:
Multiplexed Immunoassays: Platforms such as Meso Scale Discovery (MSD) employ electrochemiluminescence detection, offering up to 100-fold greater sensitivity than traditional ELISA with broader dynamic range [8]. These systems enable simultaneous quantification of multiple enzyme biomarkers in small sample volumes (25-50 μL), enhancing efficiency while reducing costs by approximately 70% compared to individual ELISAs [8].
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS): This technology provides exceptional specificity and sensitivity for low-abundance enzyme detection, enabling analysis of hundreds to thousands of proteins in single runs while avoiding antibody-dependent limitations of immunoassays [8].
Activity-Based Detection Methods: Many novel enzymes are quantified through functional assays measuring catalytic activity. For example, G6PD activity measurement serves as a biomarker for gastric cancer progression and leukemias, while acetylcholinesterase activity assays are utilized in neurodegenerative disease diagnostics [5].
Clinical Validation Study Designs
Clinical validation of novel enzyme biomarkers requires carefully structured approaches:
Case-Control Studies: Initial clinical validation typically employs case-control designs comparing biomarker levels between well-characterized patient groups and matched controls. For example, studies of carbonic anhydrase XII in pleural fluid for lung cancer diagnosis demonstrated significantly elevated levels in malignant versus benign effusions [2].
Longitudinal Monitoring Studies: Serial assessment of biomarker levels throughout disease progression and treatment response establishes monitoring utility. Research on separase in chronic myeloid leukemia employed flow cytometry to track enzyme levels over time, correlating changes with treatment response and disease progression [2].
Blinded Validation Cohorts: Independent validation in prospectively collected sample sets using predefined cutoff values is essential to minimize overfitting and establish generalizable performance characteristics.
Research Reagent Solutions for Novel Enzyme Biomarker Studies
| Research Tool Category | Specific Examples | Applications in Novel Enzyme Biomarker Research |
|---|---|---|
| Detection Substrates | AquaSpark alkaline phosphatase substrate, methylumbelliferyl phosphate [5] | Chemiluminescent and fluorogenic detection of enzyme activity in biological samples |
| Assay Platforms | MSD U-PLEX multiplex panels, LC-MS/MS systems [8] | Simultaneous quantification of multiple enzyme biomarkers with enhanced sensitivity |
| Specific Antibodies | Anti-CK-MB monoclonal antibodies, anti-TK1 antibodies [2] [5] | Immunoassay development for enzyme quantification and localization |
| Activity Assay Kits | Acetylcholinesterase assay kits, acid phosphatase assay kits [5] | Functional assessment of enzyme activity in clinical samples |
| Sample Preparation Reagents | Cell lysis buffers, protease inhibitors, protein stabilizers | Preservation of enzyme integrity in biological specimens during processing |
Technological Advances Driving Novel Enzyme Biomarker Discovery
Advanced Detection Platforms
The evolution beyond traditional ELISA methodologies to advanced platforms has significantly accelerated novel enzyme biomarker development:
Electrochemiluminescence Detection: MSD technology utilizes electrochemical stimulation of labels to emit light, providing substantially improved sensitivity and dynamic range compared to colorimetric detection [8].
Digital PCR Platforms: Enable absolute quantification of enzyme biomarkers at extremely low concentrations, particularly valuable for monitoring minimal residual disease in oncology applications [9].
Microarray Technologies: Allow parallel assessment of multiple molecular markers, transitioning from single biomarker testing to comprehensive biomarker signatures for clinical guidance [10].
Omics Technologies
High-throughput omics approaches have revolutionized enzyme biomarker discovery:
Proteomic Profiling: Mass spectrometry-based proteomics enables identification of differentially expressed enzymatic proteins across disease states [7].
Transcriptomic Analysis: RNA sequencing technologies facilitate discovery of enzyme expression patterns associated with specific pathologies [7].
Metabolomic Approaches: Measurement of metabolic fluxes provides functional readouts of enzymatic activities in physiological and disease states [7].
The field of novel enzyme biomarkers represents a dynamic interface between basic science, clinical medicine, and technological innovation. The defining characteristics of these biomarkers—enhanced specificity, mechanistic relevance, and demonstrated clinical utility—position them as powerful tools for advancing precision medicine across therapeutic areas. The rigorous validation pathway from discovery to regulatory qualification and clinical implementation ensures that truly valuable novel enzyme biomarkers meet the stringent standards required for informed clinical decision-making.
Future directions in this field include the development of increasingly multiplexed biomarker panels, integration of artificial intelligence for pattern recognition in complex enzymatic data, and the application of liquid biopsy approaches for minimally invasive disease monitoring. As detection technologies continue to evolve and our understanding of disease pathophysiology deepens, novel enzyme biomarkers will play an increasingly central role in enabling earlier diagnosis, more accurate prognosis, and personalized therapeutic strategies across a broad spectrum of human diseases.
Enzyme markers represent a cornerstone of modern clinical diagnostics and therapeutic development, serving as quantifiable indicators of biological processes, pathological states, or pharmacological responses to therapeutic intervention. These specialized biomarkers, which include specific enzymes such as 5'-nucleotidase, acetatedehydehydrogenase, neutral alpha-glucosidase, catalase, and N-acetyl-beta-glucosaminidase, provide invaluable insights into cellular function and dysfunction across a spectrum of diseases [11]. The global enzyme markers market reflects their critical importance, projected to reach approximately USD 8.5 to 25,500 million by 2032-2033, with a robust compound annual growth rate (CAGR) of 7.8% to 12.5%, fueled by increasing prevalence of chronic diseases, advancements in diagnostic technologies, and the growing emphasis on personalized medicine [11] [12].
Within the context of clinical validation research for novel biomarkers, enzymes present a compelling case for widespread adoption and continued investigation. Their unique biochemical properties—including catalytic activity, substrate specificity, and regulatable expression—position them as exceptionally sensitive and dynamic indicators of physiological homeostasis and pathological disruption. Unlike static biomarkers that provide snapshot information, enzyme biomarkers often reflect real-time functional changes within tissues and biological systems, enabling clinicians and researchers to monitor disease progression, assess therapeutic efficacy, and make informed decisions about treatment strategies [11] [7]. This article provides a comprehensive comparison of enzyme biomarkers against alternative biomarker classes, supported by experimental data and detailed methodologies relevant to researchers, scientists, and drug development professionals engaged in biomarker validation.
Comparative Analysis: Enzyme Biomarkers Versus Alternative Modalities
The selection of appropriate biomarkers is critical for successful clinical validation and eventual translation to diagnostic applications. The table below provides a systematic comparison of enzyme biomarkers against other prevalent biomarker classes, highlighting key performance characteristics and practical considerations for research and development.
Table 1: Comprehensive Comparison of Biomarker Classes for Clinical Validation Research
| Biomarker Characteristic | Enzyme Biomarkers | Genetic/DNA Methylation Biomarkers | Proteomic Biomarkers | Metabolomic Biomarkers |
|---|---|---|---|---|
| Representative Examples | 5'-nucleotidase, Catalase, N-acetyl-beta-glucosaminidase [11] | Promoter hypermethylation of tumor suppressor genes [9] | PSA, C-reactive protein | Glucose, Lactate, Cholesterol |
| Primary Biological Media | Blood, Urine, Tissue samples [11] | ctDNA from blood plasma, urine, CSF [9] | Serum, Plasma, Tissue | Serum, Plasma, Urine |
| Stability During Processing | Moderate to High (dependent on preservation conditions) | High (DNA methylation patterns remain stable) [9] | Variable (prone to degradation) | Low to Moderate (requires immediate processing) |
| Detection Methodology | Activity assays, ELISA, Spectrophotometry [12] | Bisulfite sequencing, PCR-based methods, Microarrays [9] | Immunoassays, Mass spectrometry | Mass spectrometry, NMR |
| Dynamic Range | High (catalytic amplification) | Limited to copy number | Moderate (no inherent amplification) | High (reflects metabolic flux) |
| Functional Information | Direct functional readout (catalytic activity) | Information on regulation (epigenetic control) [9] | Protein abundance | Metabolic pathway activity |
| Temporal Resolution | High (rapid response to physiological changes) | Low (represents cumulative changes) [9] | Moderate | Very High (near real-time) |
| Technical Reproducibility | High (established standardized assays) | Moderate to High (standardization improving) | Variable (antibody-dependent) | Moderate (instrument-sensitive) |
| Cost per Sample Analysis | $ | $$-$$$ | $$-$$$ | $$$ |
| Clinical Translation Potential | High (well-established in diagnostics) | Emerging (several in validation) [9] | High (widely used) | Emerging |
Enzyme biomarkers demonstrate distinct advantages in providing direct functional information through their catalytic activity, offering high temporal resolution to monitor dynamic physiological changes. Their detection often leverages catalytic amplification, enabling sensitive measurement even at low concentrations. While DNA methylation biomarkers provide valuable epigenetic information with high stability [9], and metabolomic biomarkers offer near real-time metabolic insights, enzymes strike a favorable balance between functional insight, detectability, and established clinical utility.
Table 2: Performance Metrics of Enzyme Biomarkers in Key Disease Areas
| Disease Area | Representative Enzyme Marker(s) | Sensitivity Range | Specificity Range | Key Clinical Utility |
|---|---|---|---|---|
| Liver Disease | 5'-nucleotidase, Alanine Aminotransferase | 70-90% | 85-95% | Hepatocellular damage assessment, disease monitoring |
| Cardiovascular Diseases | Creatine Kinase-MB, Troponin (protein biomarker for comparison) | 85-95% | 80-90% | Myocardial infarction diagnosis, reperfusion assessment |
| Cancer | N-acetyl-beta-glucosaminidase, Catalase [11] | 65-85% | 75-95% | Tumor subtyping, treatment response monitoring [11] |
| Neurological Disorders | Acetylcholinesterase, Neutral alpha-glucosidase [11] | 60-80% | 70-90% | Disease progression monitoring, therapeutic target |
| Metabolic Disorders | Acetate dehydrogenase [11] | 75-90% | 80-95% | Metabolic pathway assessment, treatment efficacy |
The experimental data compiled in Table 2 demonstrates that enzyme biomarkers consistently provide reliable sensitivity and specificity profiles across diverse disease areas, with particularly strong performance in metabolic and liver disorders. Their established role in clinical diagnostics underscores their reliability and translational potential compared to emerging biomarker classes that may still require extensive validation.
Experimental Protocols for Enzyme Biomarker Validation
Protocol 1: Enzyme Activity Assay for Clinical Validation
Objective: To quantitatively measure enzyme activity in biological samples for correlation with pathological states.
Materials and Reagents:
- Biological samples (serum, plasma, tissue homogenates)
- Enzyme-specific substrate solutions
- Reaction buffers (pH-optimized)
- Cofactors (NAD+, ATP, metal ions as required)
- Standard enzyme preparations (for calibration curves)
- Protein assay reagents for normalization
- Stop solution (acid, base, or inhibitor as appropriate)
Methodology:
- Sample Preparation: Homogenize tissue samples in ice-cold isotonic buffer (1:5 w/v ratio). Centrifuge at 10,000 × g for 15 minutes at 4°C. Collect supernatant for analysis. For serum/plasma, use fresh or properly stored (-80°C) samples with minimal freeze-thaw cycles.
- Reaction Mixture Assembly: In a spectrophotometric cuvette or microplate well, combine:
- 50-100 μL sample (diluted appropriately)
- 200-800 μL reaction buffer (optimal pH and ionic strength)
- 10-100 μL substrate solution (saturating concentration)
- Cofactors/inhibitors as required
- Kinetic Measurement: Incubate at 37°C while continuously monitoring absorbance/fluorescence change at appropriate wavelength for 10-30 minutes. Ensure linear reaction kinetics by verifying correlation coefficient (R² > 0.95) for product formation versus time.
- Data Analysis: Calculate enzyme activity using the molar extinction coefficient of the product. Express activity as units/mg protein or units/L sample, where one unit represents conversion of 1 μmol substrate per minute under assay conditions.
- Validation Parameters: Determine linear range, intra-assay and inter-assay precision (CV < 10%), limit of detection, and recovery efficiency (85-115%).
This standardized protocol enables reliable quantification of enzyme activity, facilitating correlation with clinical parameters and comparison across patient cohorts in validation studies.
Protocol 2: Multiplex Enzyme Analysis for Biomarker Panels
Objective: To simultaneously measure multiple enzyme activities from limited sample volumes, enabling comprehensive biomarker profiling.
Materials and Reagents:
- Multiplex assay platform (Luminex, MSD, or similar)
- Enzyme-specific capture antibodies or substrates
- Detection reagents (fluorescent, chemiluminescent, or electrochemical)
- Assay buffers and wash solutions
- Standard curves for each enzyme
- Quality control samples
Methodology:
- Plate Preparation: Coat solid phase with capture molecules specific to target enzymes or their products. Block non-specific binding sites with appropriate blocking buffer (BSA, casein, or commercial blockers).
- Sample Incubation: Add samples and standards to designated wells. Incubate with shaking (2 hours, room temperature) to facilitate binding.
- Detection Step: Add detection reagents (enzyme-specific substrates with appropriate signal-generating systems). For activity-based detection, use fluorogenic or chromogenic substrates compatible with multiplex readout.
- Signal Measurement: Read plates using appropriate instrumentation (luminescence reader, fluorescence scanner, or electrochemical detector). Ensure spectral separation for multiplex detection.
- Data Analysis: Generate standard curves for each enzyme. Calculate activities from sample signals using curve-fitting algorithms. Normalize to sample protein content or internal standards.
Multiplex approaches significantly enhance the efficiency of enzyme biomarker validation by enabling parallel assessment of multiple candidates, conserving precious clinical samples, and providing comprehensive enzymatic profiles for disease stratification.
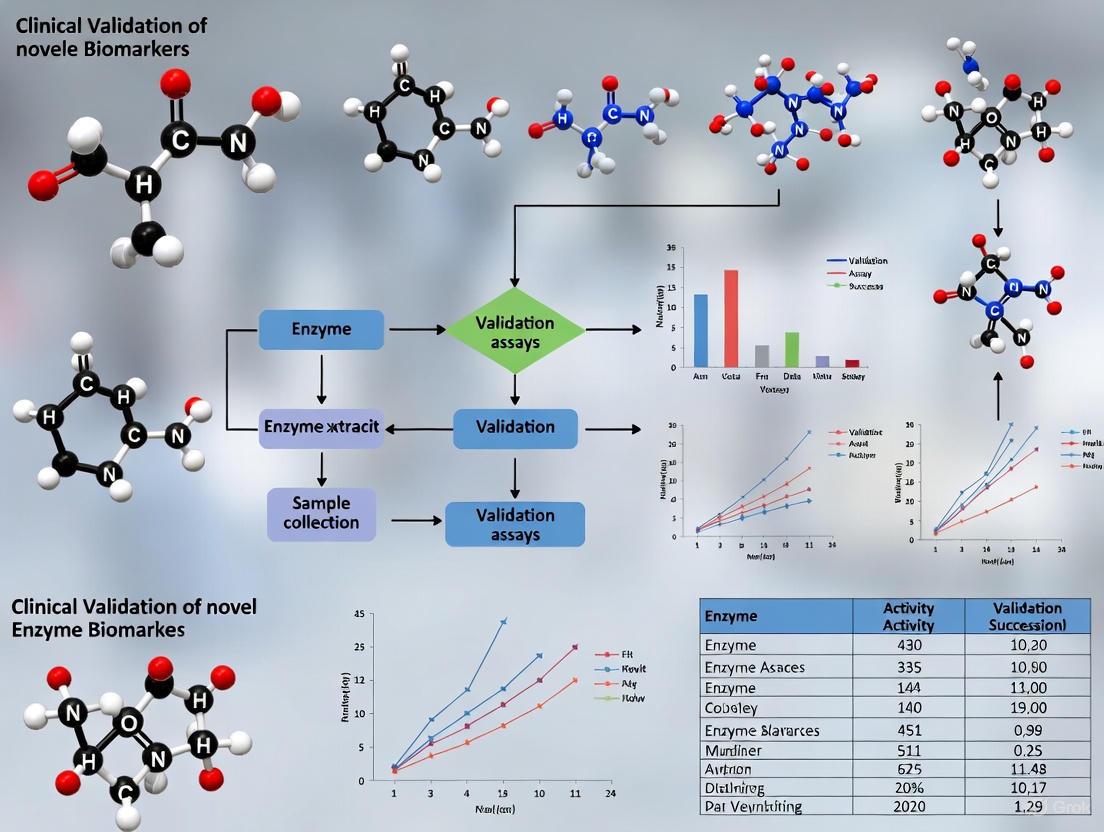
Visualizing Enzyme Biomarker Workflows and Signaling Pathways
Enzyme Biomarker Discovery and Validation Workflow
Diagram 1: Enzyme biomarker development workflow.
Enzyme-Centric Signaling Pathway Integration
Diagram 2: Enzyme biomarker pathway integration.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents for Enzyme Biomarker Investigation
| Reagent Category | Specific Examples | Primary Function | Technical Considerations |
|---|---|---|---|
| Enzyme Substrates | Chromogenic/fluorogenic substrates, Natural substrates with detection systems | Enzyme activity quantification | Selectivity, Km values, signal-to-noise ratio |
| Activity Assay Kits | Commercial enzyme activity kits (e.g., Catalase, Dehydrogenase) [12] | Standardized activity measurement | Optimization for sample matrix, linear range |
| Inhibitors/Activators | Specific chemical inhibitors, Monoclonal antibodies, Allosteric modulators | Mechanism of action studies | Specificity, concentration range, cellular toxicity |
| Detection Reagents | Antibodies, Fluorescent probes, Chemiluminescent substrates | Signal generation and amplification | Sensitivity, compatibility with instrumentation |
| Sample Preservation Solutions | Protease inhibitors, Stabilization buffers, Cryoprotectants | Pre-analytical sample integrity | Compatibility with downstream applications |
| Reference Standards | Recombinant enzymes, Calibrators, Quality control materials | Assay standardization and normalization | Purity, activity confirmation, stability |
| Solid Supports | ELISA plates, Bead-based arrays, Sensor surfaces | Immobilization and multiplexing | Binding capacity, non-specific binding |
| Signal Detection Systems | Spectrophotometers, Fluorometers, Luminescence readers [12] | Quantitative signal measurement | Dynamic range, detection limits, multiplex capability |
The selection of appropriate research reagents is critical for successful enzyme biomarker validation. Commercial assay kits provide standardized protocols and consistency across experiments [12], while custom reagent systems offer flexibility for novel enzyme targets. The trend toward immobilized enzyme reactors represents a significant technological advancement, enhancing processing efficiency and enzyme stability for repeated analyses [12].
Enzyme biomarkers present a compelling rationale for continued investigation and application in clinical validation research, offering distinct advantages as sensitive and dynamic indicators of disease states. Their capacity to provide direct functional information through catalytic activity, coupled with established detection methodologies and favorable kinetic properties, positions them as valuable tools for diagnostic development and therapeutic monitoring. The integration of enzyme biomarkers with emerging technologies—including immobilized enzyme reactors [12], advanced machine learning approaches for specificity prediction [13], and multi-omics integration strategies [7]—promises to further enhance their utility in personalized medicine and precision diagnostics.
For researchers and drug development professionals engaged in biomarker validation, enzymes represent a class of biomarkers with strong translational potential, supported by extensive clinical precedent and continuously evolving methodological refinements. Their unique combination of dynamic responsiveness, functional relevance, and detectability makes them particularly well-suited for assessing therapeutic efficacy, monitoring disease progression, and guiding treatment decisions across diverse clinical contexts. As biomarker discovery and validation methodologies continue to advance, enzyme biomarkers will undoubtedly remain essential components of the clinical diagnostics arsenal, providing critical insights into physiological and pathological processes at the molecular level.
The field of enzymology is undergoing a transformative revolution, driven by converging advances in computational biology, high-throughput screening, and bioinformatics. novel enzyme discoveries are not only expanding our understanding of biological catalysis but are also paving the way for groundbreaking applications in therapeutics, diagnostics, and industrial biotechnology. This systematic review explores the current landscape of novel enzyme discovery, focusing on the sophisticated methodologies being employed to identify and validate these biological catalysts. Within the broader thesis of clinical validation, we examine how newly discovered enzymes are progressing from initial characterization to validated biomarkers and therapeutic targets, addressing the critical pathway from discovery to clinical implementation. For researchers, scientists, and drug development professionals, understanding these emerging trends is essential for leveraging novel enzymes in diagnostic and therapeutic applications.
The significance of this field stems from the crucial roles enzymes play in health and disease. Enzymes represent a distinct class of proteins that exert specific catalytic functions within organisms, facilitating the acceleration of cellular chemical reactions and playing integral roles in biological processes including metabolism, digestion, DNA replication, and signal transduction [14]. The intricate balance of enzyme activity is vital for maintaining physiological homeostasis, and dysregulation of this balance has been implicated in the pathogenesis of numerous diseases [14]. Consequently, enzyme inhibitors have emerged as important therapeutic drugs in clinical trials, with growing research interest from fields including endocrinology, pharmacology, and toxicology [14].
Natural Products as a Primary Source
Natural products continue to serve as a rich source for novel enzyme discoveries, with distinct structural classes emerging from various organisms. A comprehensive analysis of 226 novel enzyme inhibitors isolated between 2022-2024 reveals interesting patterns in structural distribution and bioactivity prevalence [14].
Table 1: Structural Classification of Novel Enzyme Inhibitors from Natural Products (2022-2024)
| Structural Class | Percentage (%) | Representative Enzymes Targeted | Noteworthy Bioactivities |
|---|---|---|---|
| Terpenoids | 31.0 | α-Glucosidase, α-amylase, protein tyrosine phosphatase 1B | Most prevalent class; diverse skeletons |
| Flavonoids | 18.0 | α-Glucosidase, cholinesterases | Significant antioxidant properties |
| Phenylpropanoids | 14.0 | Diacylglycerol acyltransferase 1 | Includes novel sesquineolignans |
| Alkaloids | 13.0 | α-Amylase, α-glucosidase | Indole alkaloids with potent inhibition |
| Polyketides | 5.0 | Tyrosinase | Neuropyrones A-C with strong activity |
| Peptides | 4.0 | Elastase, chymotrypsin, SARS-CoV-2 3CLPro | Thiazole-containing cyclic peptides |
| Others | 15.0 | Various enzymes | Quinonoids, phenols, heptanoids |
Among these structural classes, natural products exhibiting α-glucosidase inhibitory activity are the most prevalent, accounting for 27.9% of reported compounds, followed by inhibitors targeting α-amylase and protein tyrosine phosphatase 1B [14]. This distribution reflects the ongoing search for therapeutic interventions for metabolic disorders including diabetes and obesity.
Novel Enzymes from Gut Microbiota
The human gut microbiome has emerged as a fertile ground for novel enzyme discovery. A recent groundbreaking study identified a novel β-galactosidase enzyme (Bxy_22780) in the gut bacterium Bacteroides xylanisolvens that specifically targets unique galactose-containing glycans with potential prebiotic properties [15]. Unlike typical β-galactosidases, this enzyme exclusively targets galactooligosaccharides with β-1,2-galactosidic linkages, a specificity conferred by its unique structural architecture that perfectly positions substrates for breaking down these particular sugar chains [15]. This discovery highlights the potential for novel enzymes from gut microbiota to contribute to improved human gut health and the development of new therapeutic applications.
Computational and High-Throughput Approaches
Generative Models for Enzyme Design
The field of enzyme discovery has been revolutionized by computational approaches that generate novel enzyme sequences. Three contrasting generative models have shown particular promise:
- Ancestral Sequence Reconstruction (ASR): A phylogeny-based statistical model that traverses backward in evolution, often resulting in stabilized enzyme variants [16].
- Generative Adversarial Networks (ProteinGAN): A convolutional neural network with attention trained to generate novel functional sequences [16].
- Protein Language Models (ESM-MSA): Transformer-based models that generate new sequences via iterative masking and sampling from multiple sequence alignments [16].
Experimental validation of these computational approaches has revealed important insights. In a landmark study evaluating over 500 natural and generated sequences, researchers found that initial "naive" generation resulted in mostly inactive sequences, with only 19% of tested sequences showing activity above background levels [16]. However, ASR demonstrated superior performance, generating 9 of 18 active enzymes for copper superoxide dismutase and 10 of 18 for malate dehydrogenase [16]. This highlights both the promise and current limitations of computational enzyme design.
Diagram 1: Computational enzyme discovery and validation workflow. The COMPSS computational filter improved experimental success rates by 50-150% by evaluating sequences using alignment-based, alignment-free, and structure-based metrics [16].
Deep Learning for Kinetic Parameter Prediction
Accurate prediction of enzyme kinetic parameters is crucial for efficient enzyme exploration and modification. The CataPro deep learning model represents a significant advancement in predicting turnover number (k~cat~), Michaelis constant (K~m~), and catalytic efficiency (k~cat~/K~m~) [17]. This framework utilizes embeddings from pretrained protein language models (ProtT5) and molecular fingerprints (MolT5 embeddings and MACCS keys) to create robust predictions with enhanced accuracy and generalization capability compared to previous models [17].
The practical application of CataPro was demonstrated in an enzyme mining project where researchers identified an enzyme (SsCSO) with 19.53 times increased activity compared to the initial enzyme, subsequently engineering it to improve activity by an additional 3.34-fold [17]. This success highlights the transformative potential of deep learning approaches in accelerating both enzyme discovery and optimization.
Experimental Validation and Methodologies
Benchmarking Enzyme Activity
Rigorous experimental validation remains the cornerstone of novel enzyme discovery. Standardized protocols have been developed to assess the functionality of computationally generated enzymes:
Expression and Purification Protocol:
- Gene Cloning: Genes encoding novel enzyme variants are cloned into expression vectors optimized for industrial organisms like Escherichia coli [16].
- Protein Expression: Sequences are expressed in heterologous systems, with careful attention to potential issues including codon usage hindering expression [16].
- Purification: Recombinant proteins are purified using affinity chromatography techniques [16].
Activity Assay Conditions:
- Multimeric Enzymes: For complex proteins active as multimers (e.g., malate dehydrogenase and copper superoxide dismutase), activity is assessed using spectrophotometric readouts [16].
- Success Criteria: A protein is considered experimentally successful if it can be expressed and folded in E. coli and demonstrates activity above background in in vitro assays [16].
Table 2: Key Research Reagent Solutions for Novel Enzyme Validation
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Expression Systems | Escherichia coli | Heterologous protein production | Codon optimization; avoidance of signal peptides |
| Activity Assays | Spectrophotometric enzyme assays | Quantifying catalytic function | Validation against background signals |
| Antibody Reagents | Polyclonal and monoclonal antibodies | ELISA development for biomarker validation | Epitope selection for native protein recognition |
| Analytical Platforms | Liquid chromatography-mass spectrometry (LC-MS) | Detecting enzymatic reaction products | Essential for complex reaction monitoring |
| Stability Reagents | Protease inhibitors, stabilizers | Preserving biomarker integrity during storage | Critical for clinical translation |
Biomarker Validation Workflows
The clinical validation of novel enzyme biomarkers requires carefully orchestrated workflows, particularly when developing new immunoassays. A comprehensive workflow for ELISA development encompasses four critical phases [18]:
- Antibody Production: Including careful epitope selection and specificity testing
- ELISA Development: Optimizing antibody pairs and assay conditions
- ELISA Validation: Following established guidelines (e.g., JPND-BIOMARKAPD)
- Biomarker Clinical Assessment: Large cohort analysis and multi-center studies
This structured approach is essential for overcoming the significant challenge that while global protein profiling by mass spectrometry-based proteomics has identified an enormous number of biomarker candidates, most have not been validated, hampering their implementation in clinical practice [18].
Diagram 2: Biomarker validation workflow from discovery to clinical implementation. The process involves coordinated stages from initial discovery through assay development and final clinical validation [18].
Clinical Translation of Novel Enzyme Biomarkers
Emerging Enzyme Biomarkers in Clinical Trials
The translation of novel enzyme discoveries into clinically useful biomarkers represents a critical frontier in diagnostic medicine. A systematic review of studies from 2012-2023 identified 42 eligible articles reporting novel enzymes as potential biomarkers for various conditions [2]. These emerging biomarkers can be categorized into three primary applications:
- Tumor/Cancer Biomarkers: Including carbonic anhydrase XII for small cell lung cancer, focal adhesion kinase for acute myeloid leukemia, and thymidine kinase 1 for breast cancer [2].
- Tissue and Organ Function Assessment: Such as neutrophil elastase for microvascular complications in type 2 diabetes and matrix metalloproteinase 9 for intracerebral hemorrhage prognosis [2].
- Other Disease Conditions: Enzymes that assess medical conditions not confined to specific organs [2].
Most of these novel enzyme biomarkers belong to the hydrolase class and are measured primarily by methods that incorporate immunoassay principles, reflecting the need for standardized, reproducible detection methods suitable for clinical settings [2].
Validation Challenges and Considerations
The path from novel enzyme discovery to clinically validated biomarker is fraught with challenges that must be systematically addressed:
Analytical Validation Requirements:
- Assay Imprecision and Bias: Documentation of three types of imprecision—within-run, between-run, and total imprecision—is essential for interpreting results accurately [19].
- Blood Collection Considerations: Detection of circulating biomarkers begins with appropriate blood collection tubes and processing methods, as different anticoagulants (heparin, EDTA, citrate) can significantly affect results [19].
- Standardization and Harmonization: Development of reference methods and accepted reference materials enables results from different tests to be comparable across laboratories and over time [19].
Clinical Trial Design: Two principal objectives guide clinical trials of in vitro diagnostic devices: FDA clearance and documentation of the test's value in clinical practice. Trials aimed at regulatory approval typically follow the 510(k) route requiring demonstration of "non-inferiority" compared to existing tests [19]. Appropriate patient population selection is crucial, as enrolling individuals who are too healthy or too sick can compromise the trial's ability to demonstrate clinical value [19].
The landscape of novel enzyme discovery is rapidly evolving, propelled by synergistic advances in computational design, structural biology, and high-throughput experimentation. The integration of deep learning models like CataPro for kinetic parameter prediction with traditional experimental methods represents a powerful paradigm for accelerating both enzyme discovery and engineering [17]. Similarly, the development of computational filters such as COMPSS that improve experimental success rates by 50-150% demonstrates the growing sophistication of in silico prediction tools [16].
For clinical applications, the continued identification and validation of enzyme biomarkers holds promise for addressing unmet diagnostic needs across a spectrum of diseases. As the field progresses, several key trends are likely to shape future research:
- Multimarker Strategies: Combining multiple enzyme biomarkers to improve diagnostic and prognostic accuracy for complex diseases.
- Point-of-Care Applications: Development of rapid, simplified detection methods for novel enzyme biomarkers to enable decentralized testing.
- Personalized Medicine Approaches: Leveraging enzyme polymorphisms and individual metabolic variations to tailor therapeutic interventions.
In conclusion, the systematic exploration of novel enzymes through integrated computational and experimental approaches is yielding unprecedented opportunities for therapeutic development, diagnostic advancement, and industrial application. As validation methodologies become more sophisticated and computational predictions more accurate, the translation of these discoveries into clinically impactful tools is expected to accelerate, ultimately enhancing our ability to diagnose, monitor, and treat human diseases with greater precision and efficacy. The ongoing collaboration among researchers, clinicians, and industry stakeholders will be crucial for realizing the full potential of these novel enzyme discoveries in improving human health.
In the realm of drug development and clinical diagnostics, biomarkers serve as indispensable tools that provide a measurable window into biological processes, pathological states, or pharmacological responses to therapeutic interventions. As defined by the National Institutes of Health, a biomarker is "a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention" [4]. The clinical validation of novel enzyme biomarkers represents a critical pathway for advancing precision medicine, enabling earlier disease detection, more accurate prognosis, and improved therapeutic monitoring across diverse medical conditions.
The journey from understanding a biological mechanism to establishing a validated clinical marker requires rigorous scientific framework. This process begins with comprehending the fundamental role of enzymes in physiological and pathological processes, then systematically validating their measurement in accessible biological fluids, and ultimately demonstrating clinical utility for specific contexts of use. Enzymes, as biological catalysts with high substrate specificity, are particularly valuable as biomarkers since their activity in biological fluids can provide crucial information about the source and severity of cell and tissue damage [2]. This guide objectively compares emerging enzyme biomarkers against established alternatives, providing researchers and drug development professionals with experimental data and methodological frameworks to advance the field of clinical enzymology.
Biomarker Classification and Regulatory Framework
Categorical Distinctions of Clinical Biomarkers
Biomarkers are systematically categorized based on their clinical applications, with each category serving distinct purposes in the diagnostic and therapeutic pipeline. According to established clinical frameworks, biomarkers are classified into five primary types: (i) antecedent biomarkers that identify disease risk susceptibility; (ii) screening biomarkers for detecting subclinical disorders; (iii) diagnostic biomarkers for confirming manifest diseases; (iv) staging biomarkers for categorizing disease severity; and (v) prognostic biomarkers for predicting disease course, including recurrence and therapeutic response [4]. This classification system provides a structured approach for biomarker development and validation, ensuring that each biomarker is appropriately evaluated for its intended use context.
The clinical validity and utility of a biomarker depend fundamentally on its sensitivity, specificity, predictive values, and the precision with which it can be quantified [4]. For a biomarker to achieve regulatory acceptance and clinical adoption, it must demonstrate reliability, reproducibility, and feasibility across diverse patient populations. The validation process requires careful consideration of the biomarker's biological rationale, analytical performance, and clinical correlation, with regulatory guidelines continually evolving to ensure robust evidence-based evaluation.
Regulatory Pathways for Biomarker Qualification
The qualification of novel biomarkers for specific contexts of use represents a critical milestone in translational research. Regulatory agencies including the U.S. Food and Drug Administration (FDA) have established formal biomarker qualification programs to evaluate and endorse biomarkers for defined applications in drug development [6]. This regulatory pathway typically requires extensive validation across multiple sites, demonstration of analytical robustness, and compelling evidence of clinical utility for the proposed context of use.
The recent qualification of glutamate dehydrogenase (GLDH) as a biomarker for detecting drug-induced liver injury (DILI) in clinical trials exemplifies this process. After more than a decade of collaborative research led by the Predictive Safety Testing Consortium (PSTC), the FDA qualified GLDH specifically for detecting liver injury in patients with muscle disease or suspected muscle degeneration—a population where traditional liver enzymes like ALT and AST are confounded by muscle-specific expression [6]. This achievement highlights the importance of strategic collaboration among academia, industry, and regulatory agencies in advancing biomarker science.
Figure 1: Clinical Biomarker Validation Pathway from Biological Rationale to Adoption
Established vs. Novel Enzyme Biomarkers: Comparative Analysis
Limitations of Conventional Enzyme Biomarkers
Traditional enzyme biomarkers, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), and creatine kinase (CK), have formed the cornerstone of clinical diagnostics for decades. These enzymes are routinely measured for assessing tissue damage in specific organ systems—ALT and AST for hepatic injury, and CK for muscle damage [2]. However, significant limitations have emerged with these conventional biomarkers, particularly regarding tissue specificity and diagnostic accuracy in complex clinical scenarios.
The case of ALT illustrates these limitations effectively. While ALT has served as the standard biomarker for detecting liver injury for decades, its specificity is compromised by its presence in muscle tissue. This limitation becomes particularly problematic in patient populations with concurrent muscle disease, such as Duchenne muscular dystrophy, where elevated ALT levels may reflect muscle damage rather than hepatotoxicity [6]. This lack of specificity can lead to misinterpretation of drug safety data in clinical trials and potentially inappropriate clinical management decisions. Similar limitations exist for other established enzyme biomarkers, creating a compelling need for more specific alternatives.
Emerging Novel Enzyme Biomarkers
Recent advances in enzymology and analytical technologies have enabled the discovery and validation of novel enzyme biomarkers with improved specificity and clinical utility. The table below provides a comprehensive comparison of established enzyme biomarkers alongside their novel counterparts, highlighting key advantages and validation status.
Table 1: Comparative Analysis of Established vs. Novel Enzyme Biomarkers
| Organ System | Established Biomarker | Limitations | Novel Biomarker | Advantages | Validation Status |
|---|---|---|---|---|---|
| Liver | ALT (Alanine Aminotransferase) | Non-specific; elevated in muscle disease [6] | GLDH (Glutamate Dehydrogenase) | Liver-specific; not confounded by muscle injury [6] | FDA-qualified for DILI detection in muscle disease patients [6] |
| Cancer | PSA (Prostate-Specific Antigen) | Limited specificity; false positives [4] | Thymidine Kinase 1 | Cellular proliferation marker; prognosis and therapy monitoring [2] | Clinical trials for breast cancer diagnosis, prognosis, therapy monitoring [2] |
| Neurological | Amyloid-β (Aβ42/40) | Requires PET or CSF; costly and invasive [20] | ptau-217 + Aβ42/40 combination | Blood-based; high accuracy for Alzheimer's pathology [20] | Clinical validation; predicts amyloid PET status with 91% sensitivity/specificity [20] |
| Hematological Malignancies | Lactate Dehydrogenase (LDH) | Non-specific; elevated in various conditions [4] | Separase | Chromosome segregation enzyme; disease progression marker in CML [2] | Flow cytometry method; prognostic applications in chronic myeloid leukemia [2] |
| Cardiovascular | Creatine Kinase (CK) | Non-specific; muscle origin [2] | Not specified in search results | Information limited | Under investigation |
The comparative data reveals a consistent pattern across organ systems: novel enzyme biomarkers address specific limitations of established markers, particularly through enhanced tissue specificity and improved correlation with pathological processes. The integration of biomarker combinations, such as the Aβ42/40 ratio with ptau-217 for Alzheimer's disease, demonstrates how multi-marker approaches can achieve diagnostic performance comparable to gold-standard methods while offering advantages in accessibility and scalability [20].
Methodological Approaches in Enzyme Biomarker Research
Analytical Techniques for Enzyme Biomarker Detection
The quantification of enzyme biomarkers employs diverse methodological approaches, each with distinct advantages for specific research and clinical applications. The selection of an appropriate analytical technique depends on factors including the enzyme's biochemical properties, required sensitivity and specificity, sample matrix, and intended throughput for clinical implementation.
Table 2: Analytical Methods for Enzyme Biomarker Detection and Validation
| Method Category | Specific Techniques | Measured Parameter | Applications | Advantages | Limitations |
|---|---|---|---|---|---|
| Immunoassays | Enzyme-Linked Immunosorbent Assay (ELISA) | Enzyme concentration or specific isoforms [2] | Quantification of carbonic anhydrase XII, focal adhesion kinase, thymidine kinase 1 [2] | High specificity; suitable for low-abundance enzymes | Measures mass rather than activity; antibody-dependent |
| Spectrophotometric Assays | Kinetic absorbance measurements | Enzyme activity via substrate conversion [2] | GLDH, γ-glutamyltransferase, thioredoxin reductase activity [2] | Direct activity measurement; continuous monitoring | Interference from sample components; substrate specificity critical |
| Separation-Based Methods | Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | Analytic ratio (Aβ42/40) with high precision [20] | Plasma Aβ42/40 ratio for Alzheimer's pathology [20] | High specificity and multiplexing capability | Technically demanding; expensive instrumentation |
| Fluorometric Assays | Fluorescence-based activity probes | Enzyme activity via fluorescent signals [2] | Caspase-3/7 activity in serum [2] | High sensitivity; suitable for low activity levels | Fluorescence interference; probe availability |
| Flow Cytometry | Cell-based analysis with fluorescent tags | Intracellular enzyme levels in specific cell populations [2] | Separase measurement in peripheral blood for CML [2] | Single-cell resolution; multiparameter analysis | Limited to cellular enzymes; complex sample processing |
The methodological landscape for enzyme biomarker analysis continues to evolve, with recent emphasis on high-throughput platforms that enable scalable clinical implementation. Mass spectrometry-based approaches, particularly liquid chromatography-tandem mass spectrometry (LC-MS/MS), have gained prominence for their ability to precisely quantify multiple biomarkers simultaneously, as demonstrated in the combined measurement of Aβ42/40 ratio for Alzheimer's disease assessment [20]. Similarly, advanced immunoassay platforms now enable robust quantification of low-abundance enzyme biomarkers with the precision required for clinical decision-making.
Experimental Workflows for Biomarker Validation
The validation of novel enzyme biomarkers follows a structured experimental pathway that progresses from analytical validation to clinical confirmation. The workflow typically begins with assay development and optimization, followed by analytical validation to establish precision, accuracy, linearity, and reference ranges. This critical phase ensures that the measurement technique itself is reliable and reproducible before proceeding to clinical studies.
The subsequent clinical validation phase examines the biomarker's performance in well-characterized patient cohorts, establishing diagnostic sensitivity and specificity, prognostic value, or utility for therapy monitoring. For example, the validation of GLDH as a specific liver injury biomarker involved comparative studies in patients with and without muscle disease, demonstrating its superiority to ALT in distinguishing hepatic from muscular injury [6]. Similarly, the combination of plasma Aβ42/40, ptau-217, and APOE4 genotype was validated against amyloid PET imaging as the reference standard in a diverse cohort including patients with mild cognitive impairment and Alzheimer's disease [20].
Figure 2: Experimental Workflow for Enzyme Biomarker Analysis and Validation
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research and development of enzyme biomarkers requires carefully selected reagents and materials that ensure analytical reliability and reproducibility. The following table summarizes essential components of the biomarker researcher's toolkit, with specific examples from recent studies.
Table 3: Essential Research Reagents and Materials for Enzyme Biomarker Studies
| Reagent Category | Specific Examples | Function/Purpose | Application Examples |
|---|---|---|---|
| Biological Samples | Serum, plasma, saliva, pleural fluid [2] | Matrix for enzyme measurement; different sample types for different applications | Serum for GLDH measurement [6]; plasma for ptau-217 [20]; pleural fluid for carbonic anhydrase XII [2] |
| Antibodies | Monoclonal and polyclonal antibodies | Specific recognition and capture of target enzymes in immunoassays | ELISA for thymidine kinase 1, focal adhesion kinase [2] |
| Enzyme Substrates | Synthetic chromogenic/fluorogenic substrates | Enzyme activity measurement through product formation | Spectrophotometric substrates for GLDH, γ-glutamyltransferase [2] |
| Reference Standards | Recombinant enzymes, purified protein standards | Calibration and quantification reference | Mass spectrometry reference materials for Aβ42/40 ratio [20] |
| Sample Preparation Reagents | Protease inhibitors, stabilizers, extraction buffers | Preserve enzyme activity and structure during processing | Citrate-based anticoagulants for neutrophil elastase measurement [2] |
| Detection Reagents | Fluorescent probes, enzyme conjugates, detection antibodies | Signal generation and amplification in detection systems | Fluorometric caspase-3/7 substrates [2] |
| Separation Materials | LC columns, solid-phase extraction cartridges | Analytic separation and purification before detection | LC-MS/MS columns for Aβ42/40 measurement [20] |
The selection of appropriate reagents must align with the specific analytical platform and intended application. For example, mass spectrometry-based approaches require stable isotope-labeled internal standards for precise quantification, while immunoassays depend on high-specificity antibody pairs with minimal cross-reactivity. Similarly, sample collection materials must be carefully selected to preserve enzyme activity—certain anticoagulants can interfere with specific enzyme measurements, making standardized sample processing protocols essential for reproducible results.
The field of clinical enzymology continues to evolve rapidly, driven by advances in analytical technologies, improved understanding of disease mechanisms, and growing recognition of the need for more specific biomarkers. The comparative data presented in this guide demonstrates a clear trend toward tissue-specific enzymes that provide more accurate diagnostic and prognostic information compared to conventional markers. The successful regulatory qualification of GLDH for specific contexts of use establishes an important precedent for future biomarker development and highlights the value of collaborative consortia in advancing the field.
Future directions in enzyme biomarker research will likely focus on several key areas: First, the development of multi-marker algorithms that combine multiple enzymes or integrate enzymes with other biomarker classes (e.g., proteins, genetic markers) to achieve superior diagnostic performance, as exemplified by the combination of Aβ42/40, ptau-217, and APOE genotype for Alzheimer's disease [20]. Second, the continued refinement of high-throughput analytical platforms that enable cost-effective, scalable implementation in clinical practice. Third, the exploration of novel enzyme classes beyond traditional hydrolases and transferases, potentially including specialized enzymes from specific pathological processes.
As the biomarker landscape evolves, researchers and drug development professionals must maintain rigorous standards for analytical validation and clinical demonstration of utility. Through continued collaboration across academia, industry, and regulatory agencies, the translation of novel enzyme biomarkers from mechanistic insights to clinically valuable tools will accelerate, ultimately enabling more precise diagnosis, effective therapy selection, and improved patient outcomes across diverse disease areas.
In the era of precision medicine, biomarkers serve as critical measurable indicators for understanding biological processes, pathological states, and responses to therapeutic interventions [21]. Enzyme biomarkers, as biological catalysts, are particularly valuable due to their substrate specificity and the ability to relate their activity to concentration in biological fluids, providing vital information on the source and severity of cell and tissue damage [2]. The clinical utility of these biomarkers is defined by their specific intent: diagnostic biomarkers identify the presence of a disease, prognostic biomarkers forecast the natural course of a disease, predictive biomarkers estimate the likelihood of response to a specific treatment, and monitoring biomarkers are used to track disease status or treatment response over time [21]. This guide objectively compares the performance of novel and established enzyme biomarkers across these clinical intents, providing researchers and drug development professionals with a data-driven resource for clinical validation.
Comparison of Enzyme Biomarker Applications
The table below summarizes the clinical performance of various enzyme biomarkers, highlighting their specific applications and key performance metrics.
Table 1: Clinical Applications and Performance of Select Enzyme Biomarkers
| Enzyme Biomarker | Clinical Intent | Associated Disease/Condition | Specimen | Key Performance Data |
|---|---|---|---|---|
| Thymidine Kinase 1 [2] | Diagnosis, Prognosis, Monitoring | Breast Cancer | Serum | Used for diagnosis, prognosis, and therapy monitoring (Method: ELISA) |
| Caspase-3/7 [2] | Prognosis, Monitoring | Head and Neck Squamous Cell Carcinoma | Serum | Prognosis and therapy monitoring (Method: Fluorometry) |
| γ-glutamyltransferase (GGT) [2] | Prognosis | Advanced Urothelial Cancer | Serum | Serves as a prognostic indicator (Method: Spectrophotometry) |
| Focal Adhesion Kinase (FAK), Src, PKC [2] | Diagnosis, Prognosis | Acute Myeloid Leukemia (AML) | Serum | Used for diagnosis and prognosis (Method: ELISA) |
| Lactate Dehydrogenase (LDH) [22] [2] | Diagnosis, Prognosis | Brainstem Glioma (BSG), Various Cancers | Serum, Saliva | Diagnostic model for BSG achieved an AUC of 0.933 in an independent blind test [22] |
| 2-Deoxy-D-Glucose (2-DG) [23] | Predictive (Therapy Candidate) | Cancer (Glycolysis Inhibition) | N/A (Research Compound) | Used in enzyme kinetics studies to inhibit cancer cell metabolism; evaluated as an adjunct therapy |
| Neutrophil Elastase [2] | Prognosis | Type 2 Diabetes Microvascular Complications | Citrated Plasma | Serves as a prognostic indicator for complications (Method: ELISA) |
| Alanine Transaminase (ALT) [24] | Monitoring | Post-COVID-19 Liver Function | Serum | Levels showed a significant difference (p=0.002) between mild and severe post-COVID-19 cases |
Experimental Protocols for Biomarker Evaluation
Protocol for Serum-Based Metabolic Profiling in Brainstem Glioma
This protocol, used to identify diagnostic and prognostic metabolic enzyme biomarkers, is based on a study of brainstem gliomas (BSG) [22].
- Objective: To distinguish BSG patients from healthy donors (HDs) and predict patient survival using static and dynamic serum metabolic snapshots.
- Specimen Collection: Collect serum from a well-characterized patient cohort (e.g., 106 BSG patients and HDs). For dynamic monitoring, perform high-density, three-weekly blood draws prior to and during radiotherapy.
- Metabolite Profiling:
- Technology: Employ Nanoparticle-Enhanced Laser Desorption/Ionization Mass Spectrometry (NPELDI-MS).
- Procedure: Use ferric nanoparticles to enrich metabolites from native serum inputs (as small as 0.1 μL) without pretreatment. Analyze samples with a laser pulse frequency of 1000 Hz (approx. 2 seconds per sample).
- Data Analysis:
- Process raw MS spectra (e.g., 120,000 data points per sample) and filter features via quality control.
- Apply machine learning algorithms for diagnostic model building. Use a discovery set (e.g., n=99) for model training.
- Use shrinkage methods like LASSO (Least Absolute Shrinkation and Selection Operator) and Ridge for feature selection to identify top metabolite biomarkers (e.g., lactic acid, valine, leucine).
- Validate the classification model's performance (e.g., sensitivity, specificity, Area Under the Curve - AUC) on an independent validation set (e.g., n=34).
Protocol for Evaluating Computer-Generated Enzyme Sequences
This protocol is designed for the experimental validation of novel enzymes generated by computational models, a key step in biomarker and therapeutic development [16].
- Objective: To assess whether in silico-generated enzyme sequences are expressed, fold correctly, and are functionally active.
- Sequence Generation & Selection:
- Generate novel sequences using diverse computational models (e.g., Ancestral Sequence Reconstruction - ASR, Generative Adversarial Networks - GANs, Protein Language Models).
- Apply computational filters (e.g., the COMPSS framework) to select phylogenetically diverse sequences with a high probability of being functional.
- Expression and Purification:
- Clone the selected genes into an industrial expression system like Escherichia coli.
- Express and purify the proteins using standard recombinant DNA techniques (e.g., affinity chromatography).
- Functional Activity Assay:
- Perform in vitro activity assays with a spectrophotometric readout.
- For malate dehydrogenase (MDH) and copper superoxide dismutase (CuSOD), specific biochemical assays are used to measure catalytic activity.
- Success Criterion: Define an experimentally successful protein as one that is expressed and folded in E. coli and demonstrates activity significantly above background in the in vitro assay.
Visualization of Workflows and Pathways
Biomarker Clinical Translation Pathway
The following diagram illustrates the multi-stage pathway for translating a novel biomarker from discovery to clinical application, integrating key challenges and processes.
Experimental Validation Workflow
This flowchart details the key steps and decision points in the experimental protocol for validating novel enzyme biomarkers or generated enzyme sequences.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table lists essential reagents and technologies used in the development and validation of enzyme biomarkers, as featured in the cited experimental protocols.
Table 2: Essential Reagents and Technologies for Enzyme Biomarker Research
| Research Reagent / Technology | Primary Function in Research | Experimental Context |
|---|---|---|
| U-PLEX Multiplexed Immunoassay Platform (MSD) [8] | Simultaneously measure multiple enzyme/protein biomarkers from a single, small-volume sample. | Used for efficient biomarker validation; offers superior sensitivity and a broader dynamic range compared to traditional ELISA. |
| NPELDI-MS(Nanoparticle-Enhanced LDI-MS) [22] | Pretreatment-free mass spectrometry for high-speed, high-throughput metabolic profiling using trace serum samples. | Employed to acquire comprehensive static and dynamic metabolic snapshots for diagnostic and prognostic model building. |
| LASSO & Ridge Regression [22] [21] | Machine learning-based feature selection methods to identify the most relevant biomarker combinations from high-dimensional data. | Critical for selecting optimal metabolic features (e.g., lactic acid, valine) to build parsimonious and effective diagnostic models. |
| COMPSS Framework(Composite Metrics for Protein Sequence Selection) [16] | A computational filter combining multiple metrics to predict the in vitro activity of computer-generated enzyme sequences. | Used to select phylogenetically diverse, functional enzyme sequences for experimental testing, improving success rates by 50-150%. |
| ESM-MSA, ProteinGAN, ASR Models [16] | Diverse generative models (Language Model, GAN, Ancestral Sequence Reconstruction) to create novel enzyme sequences. | Utilized to explore functional sequence diversity beyond natural proteins for novel biocatalyst and biomarker development. |
Advanced Assay Development and Strategic Application in Clinical Trials
The clinical validation of novel enzyme biomarkers demands analytical platforms that deliver uncompromising sensitivity, specificity, and precision. For decades, Enzyme-Linked Immunosorbent Assay (ELISA) has been the workhorse technique in biomolecular analysis, valued for its simplicity, cost-effectiveness, and versatility in detecting specific proteins [25]. However, the emergence of precision medicine and the need to detect lower abundance biomarkers in complex matrices have revealed ELISA's limitations, including antibody cross-reactivity, limited dynamic range, and insufficient sensitivity for trace-level detection [25] [8].
Advanced platforms such as Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) and Meso Scale Discovery (MSD) are increasingly becoming the preferred choices for rigorous biomarker validation. These technologies offer transformative improvements in sensitivity, specificity, and multiplexing capabilities, enabling researchers to obtain more reliable and actionable data from precious clinical samples [8] [26]. This shift is further supported by evolving regulatory standards that emphasize more comprehensive validation data, including enhanced analytical validity and cross-validation techniques [27] [26]. This guide provides an objective comparison of these advanced platforms against traditional ELISA to inform method selection for enzyme biomarker research.
Technology Platform Comparisons
Fundamental Principles and Mechanisms
ELISA (Enzyme-Linked Immunosorbent Assay) operates on the principle of antibody-antigen interaction, where the detection of a target molecule is achieved through an enzymatic reaction that produces a colorimetric, fluorescent, or chemiluminescent signal. Its performance is heavily dependent on the quality and specificity of the antibody reagents used [25] [8].
LC-MS/MS (Liquid Chromatography-Tandem Mass Spectrometry) combines two powerful analytical techniques. Liquid chromatography first separates the components of a complex biological sample, which are then ionized and introduced into the mass spectrometer. The tandem mass spectrometer then precisely identifies and quantifies molecules based on their mass-to-charge ratio and characteristic fragmentation patterns [25] [28]. This method provides direct, molecule-by-molecule analysis, enabling the identification and quantification of biomolecules with high specificity.
MSD (Meso Scale Discovery) technology is an electrochemiluminescence-based detection method that shares similarities with ELISA in its use of antibody-antigen interactions. However, instead of colorimetric detection, MSD uses sulfo-tag labels that emit light upon electrochemical stimulation at the surface of electrodes embedded in the plate wells [29] [30]. This fundamental difference in detection methodology confers significant advantages in sensitivity and dynamic range.
Comparative Technical Specifications
Table 1: Technical comparison between ELISA, LC-MS/MS, and MSD platforms
| Feature | ELISA | LC-MS/MS | MSD |
|---|---|---|---|
| Principle | Antibody-antigen interaction with colorimetric detection | Separation by chromatography and mass-based detection | Antibody-antigen interaction with electrochemiluminescence detection |
| Sensitivity | Good for moderate concentrations | Excellent for trace-level detection (e.g., LOQ of 0.1 ng/mL for cotinine) [28] | High sensitivity (up to 100x greater than ELISA) [8] |
| Dynamic Range | 1-2 logs [29] | 3-4+ logs [25] | 3-4+ logs [29] [30] |
| Sample Volume Requirement | 50-100 μL (per analyte) [29] | Varies with method, typically low | 10-25 μL (for up to 10 analytes) [29] |
| Multiplexing Capability | Limited to single-plex | Moderate (requires method development) | High (up to 10 analytes simultaneously) [29] |
| Specificity | Can be affected by cross-reactivity [25] | Highly specific, distinguishes molecular isoforms [25] | High, with reduced cross-reactivity |
| Throughput | Moderate | Lower (multistep process) | High (fast read times: 1-3 minutes per plate) [29] |
| Matrix Effects | Susceptible to interference | Minimized through separation | Greatly reduced [29] [30] |
Experimental Data and Performance Comparison
Quantitative Performance in Biomarker Detection
Direct comparative studies demonstrate the superior performance of advanced platforms in actual biomarker measurement applications:
Table 2: Experimental performance data comparing ELISA and LC-MS/MS for cotinine detection in children's saliva [28]
| Parameter | LC-MS/MS | ELISA |
|---|---|---|
| Limit of Quantitation (LOQ) | 0.1 ng/mL | 0.15 ng/mL |
| Geometric Mean (GeoM) of Cotinine | 4.1 ng/mL | 5.7 ng/mL |
| Range | ||
| Samples |
3% | 5% |
| Revealed Significant Associations | With sex and race/ethnicity | No significant associations with sex or race/ethnicity |
The study demonstrated that utilizing LC-MS/MS-based cotinine measurement revealed associations with sex and race/ethnicity of children that were not detectable using ELISA-based cotinine, highlighting the benefits of utilizing more sensitive assays when detecting low levels of exposure [28].
Correlation Between Methods
A 2025 study comparing isotope-dilution LC-MS/MS and a newly established ELISA for desmosine (an elastin degradation biomarker) found that while both methods exhibited a high correlation coefficient (0.9941), the ELISA measurements ranged from 0.83 to 1.06 times the theoretical values, whereas LC-MS/MS measurements initially showed approximately 2-fold deviations [31]. After recalibration using a corrected molar extinction coefficient, the LC-MS/MS measurements ranged from 0.68 to 0.99 times the theoretical values, demonstrating that both methods can achieve high accuracy with proper standardization [31].
Detailed Experimental Protocols
LC-MS/MS Methodology for Biomarker Quantification
The following workflow details a standardized approach for LC-MS/MS analysis of enzyme biomarkers, based on protocols used in comparative studies:
LC-MS/MS Workflow for Biomarker Analysis
Sample Preparation Protocol:
- Internal Standard Addition: Add a known quantity of isotopically-labeled internal standard (e.g., 10 μL of 100 ppm isodesmosine-13C3,15N1) to 0.2 mL of sample to correct for variability in sample preparation and analysis [31].
- Protein Precipitation: Add organic solvents (e.g., acetonitrile or methanol) to remove proteins and other interfering compounds.
- Solid-Phase Extraction (SPE): Pass samples through conditioned SPE cartridges to concentrate analytes and remove additional matrix components [28].
Hydrolysis and Cleanup (for protein-bound biomarkers):
- Acid Hydrolysis: Heat samples with 6M HCl at 110°C for 16-24 hours to release protein-bound biomarkers [31].
- Cellulose Column Purification: Remove impurities using a cellulose column after hydrolysis. Wash with 3 mL of 1-butanol/acetic acid/H2O (4:1:1) three times, then elute target analytes with 3 mL of H2O [31].
LC-MS/MS Analysis:
- Chromatographic Separation: Use a C18 column (e.g., Luna C18) with gradient elution (typically water/acetonitrile with 0.1% formic acid) to separate analytes prior to mass spectrometry [28].
- Mass Spectrometric Detection: Operate in Multiple Reaction Monitoring (MRM) mode, selecting specific precursor-to-product ion transitions for each biomarker and its internal standard.
- Quantitation: Generate calibration curves using the area ratio of analyte to internal standard, ensuring linearity with R² values >0.99 [31].
MSD Electrochemiluminescence Immunoassay Protocol
MSD Assay Workflow
Assay Procedure:
- Plate Preparation: Use MSD MULTI-ARRAY plates containing carbon electrode surfaces. Coat plates with capture antibody specific to the target biomarker (1-10 μg/mL in PBS overnight at 4°C) [30].
- Blocking: Block plates with 150 μL of blocking buffer (e.g., 3% BSA in PBS with 0.05% Tween-20) for 1-2 hours at room temperature with shaking.
- Sample Incubation: Add samples and standards (10-25 μL volume) to wells and incubate for 2 hours with shaking. MSD requires significantly less sample volume than ELISA - typically 10-25 μL for up to 10 analytes compared to 50-100 μL per analyte for ELISA [29].
- Detection Antibody Incubation: Add sulfo-tag labeled detection antibody and incubate for 1-2 hours with shaking.
- Signal Detection: Add MSD Read Buffer and measure electrochemiluminescence signal using an MSD instrument (e.g., QuickPlex SQ 120). The instrument applies an electrical potential to the plate electrodes, exciting the sulfo-tag labels to emit light [30].
Multiplex Assay Configuration: For multiplex panels such as cytokine measurements, use MSD's U-PLEX technology, which allows simultaneous measurement of multiple biomarkers from a single sample. This approach significantly reduces costs compared to multiple ELISAs - for example, measuring four inflammatory biomarkers (IL-1β, IL-6, TNF-α, and IFN-γ) costs approximately $19.20 per sample with MSD versus $61.53 per sample with individual ELISAs [8].
Essential Research Reagent Solutions
Table 3: Key research reagents and materials for advanced biomarker detection platforms
| Reagent/Material | Function | Platform Application |
|---|---|---|
| Isotopically-Labeled Internal Standards | Correct for sample preparation and ionization variability; enable precise quantitation | LC-MS/MS |
| Sulfo-Tag Conjugated Antibodies | Generate electrochemiluminescence signal upon electrical stimulation | MSD |
| Carbon Electrode Microplates | Provide surface for antibody immobilization and electrochemical stimulation | MSD |
| Solid-Phase Extraction Cartridges | Concentrate analytes and remove matrix interference prior to analysis | LC-MS/MS |
| Mobile Phase Additives (Formic Acid, Ammonium Acetate) | Modify chromatography and enhance ionization efficiency | LC-MS/MS |
| Multiplex Capture Spots | Enable simultaneous measurement of multiple analytes in a single well | MSD (U-PLEX) |
| High-Affinity, High-Specificity Antibody Pairs | Ensure specific capture and detection of target biomarkers with minimal cross-reactivity | MSD, ELISA |
Regulatory and Practical Implementation Considerations
Regulatory Landscape
Recent regulatory developments emphasize the need for more rigorous biomarker validation methods. The FDA's 2025 Bioanalytical Method Validation for Biomarkers guidance directs sponsors to apply ICH M10 criteria when submitting biomarker data associated with regulatory approvals [27] [26]. This guidance highlights the importance of:
- Context of Use (COU): While not explicitly referenced in the FDA guidance, the European Bioanalytical Forum has emphasized that biomarker validation must consider the specific intended use [27].
- Parallelism Assessments: Demonstrating that the dilution-response curve of the sample parallels the standard curve, particularly when using surrogate matrices [27].
- Specificity and Sensitivity: Addressing frequent issues that lead to rejection, including problems with specificity, sensitivity, detection thresholds, and reproducibility [8].
Strategic Platform Selection
When implementing advanced platforms for enzyme biomarker validation, consider these strategic factors:
Choose LC-MS/MS when:
- Ultra-high sensitivity is required for trace-level detection [25]
- Specific distinction between molecular isoforms or post-translational modifications is needed [25]
- Dealing with complex matrices where antibody-based methods show interference [28]
- Measuring small molecules or metabolites alongside protein biomarkers [28]
Select MSD when:
- Multiplexing capability is important for measuring biomarker panels [29] [8]
- Sample volume is limited (requires only 10-25 μL for multiple analytes) [29]
- Higher throughput is needed with minimal sample preparation [30]
- Enhanced sensitivity over ELISA is required without LC-MS/MS complexity [8]
Consider ELISA when:
- Analyzing high-abundance biomarkers with well-established antibodies [25]
- Budget constraints are significant and equipment access is limited [25]
- Single-plex measurements are sufficient for study objectives [26]
- Method simplicity and widespread availability are priorities [26]
The implementation of advanced platforms requires careful consideration of the balance between precision, sensitivity, cost, and regulatory requirements. As noted in recent industry analysis, "Precision is paramount in biotech applications because it impacts data turnaround times, cost-efficiency, and experimental repeats" [26]. By selecting the appropriate platform based on the specific validation requirements and context of use, researchers can generate the robust, reproducible data needed to advance biomarker discovery and qualification.
Best Practices for Developing and Validating Robust Enzymatic Activity Assays
Enzymatic activity assays serve as fundamental tools in drug discovery and development, particularly in the clinical validation of novel enzyme biomarkers. These assays provide critical data on enzyme kinetics, inhibition, and target engagement, supporting decisions from early screening to late-stage clinical trials. This guide examines best practices for developing robust enzymatic assays, compares modern detection technologies, and outlines experimental protocols for ensuring data quality and reproducibility. Within the framework of clinical biomarker validation, we explore how rigorous enzymatic profiling underpins the qualification of pharmacodynamic biomarkers and the assessment of therapeutic efficacy for enzyme-targeting drugs.
Enzymes are biological catalysts responsible for mediating essential biochemical reactions, and their dysregulation is implicated in numerous diseases including cancer, neurodegenerative conditions, and metabolic disorders [32] [33]. Enzymatic activity assays are laboratory methods designed to measure the rate at which an enzyme converts its specific substrate into product, providing quantitative data on enzyme function [34] [35]. In drug discovery contexts, these assays enable researchers to identify and characterize compounds that modulate enzyme activity, forming the foundation for therapeutic development [33].
The clinical validation of enzyme biomarkers demands particularly rigorous assay development, as these biomarkers must demonstrate analytical validity, clinical validity, and utility in regulatory settings [32] [36]. Robust enzymatic assays are prerequisite tools for establishing these parameters, allowing researchers to quantify functional enzyme activity in relation to disease phenotypes, therapeutic interventions, and clinical outcomes [32]. The transition from traditional spectrophotometric methods to advanced fluorescence and luminescence-based platforms has significantly enhanced the sensitivity, throughput, and reliability required for modern biomarker validation workflows [34] [33] [8].
Fundamental Principles of Enzyme Kinetics and Assay Design
Key Kinetic Parameters
Understanding enzyme kinetics is essential for meaningful assay design and interpretation. The Michaelis-Menten model describes the relationship between substrate concentration and reaction velocity through the equation:
v = (Vmax × [S]) / (Km + [S])
Where:
- v = initial velocity of the reaction
- Vmax = maximal reaction rate when enzyme is saturated with substrate
- [S] = substrate concentration
- Km = Michaelis constant, the substrate concentration at half of Vmax [35]
The Km value represents the enzyme's affinity for its substrate, with lower values indicating higher affinity. For assay development, it is crucial to run reactions with substrate concentrations at or below the Km value when identifying competitive inhibitors [35]. The initial velocity of the reaction—measured when less than 10% of substrate has been consumed—must be determined to ensure accurate kinetic measurements before factors like product inhibition, substrate depletion, or enzyme instability influence the reaction rate [35].
Critical Factors Affecting Enzyme Activity
Multiple parameters must be carefully controlled during assay development to ensure reproducible results:
- Temperature: Enzyme activity is highly sensitive to temperature fluctuations, with just a 1°C change potentially causing 4-8% variation in measured activity. Assays should be performed with precise temperature control between 25-37°C, depending on the enzyme's optimal range and physiological relevance [34] [37].
- pH: Each enzyme has an optimal pH that maximizes its activity. pH affects the enzyme's charge conformation and substrate binding capacity. Buffer composition and ionic strength must be standardized across experiments [34].
- Enzyme Concentration: The assay must operate in the linear range where reaction velocity is directly proportional to enzyme concentration. This requires empirical determination using serial dilutions to identify the appropriate concentration window [35] [37].
- Time: Reactions should be monitored during the initial linear phase, typically between 15-60 minutes, to ensure that less than 15% of substrate has been converted to product [37].
The following diagram illustrates the key considerations and workflow for establishing robust assay conditions:
Comparison of Enzymatic Assay Detection Technologies
Multiple detection platforms are available for monitoring enzymatic activity, each with distinct advantages, limitations, and optimal use cases. The selection of an appropriate detection method depends on factors including throughput requirements, sensitivity needs, instrumentation availability, and potential interference compounds [34] [33].
Radiometric assays were historically considered the gold standard for direct detection, particularly for kinase studies, but have been largely replaced by safer alternatives due to radioactive waste concerns and limited scalability [33]. Absorbance/colorimetric assays offer simplicity and cost-effectiveness but suffer from lower sensitivity, making them less suitable for miniaturized high-throughput screening (HTS) [34] [33]. Luminescence-based methods provide excellent sensitivity and dynamic range but may be susceptible to interference from luciferase inhibitors and coupling artifacts [33].
Fluorescence-based assays have emerged as the dominant technology for HTS applications due to their superior sensitivity, compatibility with automation, and adaptability across multiple enzyme classes [34] [33]. Recent advancements in universal fluorescent detection platforms that monitor common products like ADP, GDP, or SAH offer particular versatility across diverse enzyme families including kinases, GTPases, and methyltransferases [33].
Comparative Analysis of Detection Methods
Table 1: Comprehensive Comparison of Enzymatic Assay Detection Technologies
| Assay Type | Detection Principle | Sensitivity | Throughput Potential | Key Advantages | Major Limitations | Best Applications |
|---|---|---|---|---|---|---|
| Radiometric | Radioactive decay measurement | High | Low | Direct, quantitative measurement; Historical gold standard | Radioactive waste; Safety concerns; Limited scalability | Historical standard for kinases; Metabolic enzymes |
| Fluorescence | Fluorescent signal emission | Very High | Very High (384-/1536-well) | High sensitivity; HTS compatible; Homogeneous formats possible | Potential fluorescent compound interference; Quenching effects | Universal for kinases, GTPases, helicases, methyltransferases |
| Luminescence | Light emission from enzymatic reaction | High | High (384-well) | Broad dynamic range; High sensitivity | Susceptible to luciferase inhibitors; Coupling artifacts | ATP-dependent enzymes; Kinases; Methyltransferases |
| Absorbance/Colorimetric | Optical density/color change | Low-Moderate | Moderate (96-/384-well) | Simple; Inexpensive; Robust | Lower sensitivity; Not ideal for miniaturized HTS | Early-stage validation; Educational assays |
| Label-Free (SPR, ITC) | Mass, refractive index, or heat change | Variable | Low | No label interference; Direct thermodynamic data | Low throughput; Specialized instrumentation | Mechanistic studies; Binding characterization |
For biomarker validation studies requiring high precision and reproducibility, technologies such as Meso Scale Discovery (MSD) electrochemiluminescence and LC-MS/MS are gaining traction due to their enhanced sensitivity and multiplexing capabilities compared to traditional ELISA [8]. MSD platforms offer up to 100-fold greater sensitivity than ELISA with a broader dynamic range, while LC-MS/MS enables highly specific detection of low-abundance species and complex post-translational modifications [8].
Experimental Protocols for Robust Assay Development
Determining Initial Velocity and Linear Range
Establishing initial velocity conditions is fundamental to obtaining meaningful kinetic data. The following protocol ensures accurate measurement:
- Enzyme Titration: Prepare serial dilutions of enzyme (e.g., 1:2, 1:5, or log dilutions) in reaction buffer. Include a no-enzyme control for background subtraction [35] [37].
- Time Course Experiment: For each enzyme concentration, monitor product formation at multiple time points (e.g., 0, 5, 10, 20, 30, 60 minutes) under fixed substrate concentration [35].
- Identify Linear Range: Plot product concentration versus time for each enzyme dilution. Select the time window where the relationship is linear (typically <10% substrate conversion) for all enzyme concentrations tested [35].
- Optimize Enzyme Concentration: Choose an enzyme concentration that falls within the linear range of both the time course and the detection system's capacity [35].
The reaction progress curves typically demonstrate three phases: an initial linear phase (initial velocity), a curvature phase as substrate depletes, and a plateau when the reaction completes. All kinetic measurements should be confined to the initial linear phase where steady-state assumptions remain valid [35].
Measuring Km and Vmax Values
Accurate determination of kinetic parameters ensures appropriate substrate concentrations for subsequent inhibition studies:
- Substrate Titration: Prepare a dilution series of substrate covering a range of 0.2-5.0 × the expected Km value. Use at least 8 different substrate concentrations for reliable curve fitting [35].
- Fixed Enzyme Concentration: Use a single, optimized enzyme concentration (determined in section 4.1) for all substrate concentrations.
- Initial Velocity Measurement: For each substrate concentration, measure product formation during the initial linear phase identified previously.
- Data Analysis: Plot initial velocity (v) versus substrate concentration ([S]). Fit data to the Michaelis-Menten equation using nonlinear regression to determine Km and Vmax values [35].
- Iterative Refinement: If the initial Km estimate has high uncertainty, perform a second experiment with substrate concentrations focused around the estimated Km value (e.g., 0.1-2.0 × Km) [35].
For drug discovery applications focused on competitive inhibitor identification, assays should be conducted with substrate concentrations at or below the Km value to maximize sensitivity to inhibition [35].
Validation Parameters for Clinical Biomarker Applications
Enzymatic assays supporting clinical biomarker validation must demonstrate rigorous performance characteristics:
- Accuracy and Precision: Intra- and inter-assay coefficients of variation (CV) should typically be <10-20%, depending on the clinical application [36] [8].
- Specificity: The assay should specifically measure the target enzyme activity without interference from related enzymes or matrix components.
- Linearity and Range: The analytical measurement range must encompass clinically relevant enzyme activity levels with demonstrated linearity [37].
- Robustness: Assay performance should remain consistent despite minor variations in reagent lots, operators, or instruments [32].
- Reference Standards: Include qualified reference materials or controls to enable normalization across experiments and laboratories [32].
For formal biomarker qualification, regulatory agencies including the FDA and EMA recommend a "fit-for-purpose" approach where the validation rigor corresponds to the intended clinical use [32] [8].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Enzymatic Assay Development
| Reagent Category | Specific Examples | Function and Importance | Selection Considerations |
|---|---|---|---|
| Enzyme Sources | Recombinant enzymes; Tissue/cell extracts | Catalytic component being measured | Purity, specific activity, lot-to-lot consistency, post-translational modifications |
| Substrates | Natural substrates; Peptide surrogates; Fluorogenic compounds | Molecule converted by enzyme activity | Km value, solubility, commercial availability, detection compatibility |
| Cofactors | ATP, NADH, metal ions, vitamins | Essential for catalytic activity in many enzymes | Stability, concentration optimization, potential inhibition at high levels |
| Detection Reagents | Fluorescent probes, luminescent substrates, antibody conjugates | Enable quantification of reaction products | Sensitivity, dynamic range, compatibility with HTS, interference potential |
| Buffer Components | Tris, HEPES, PBS with varying pH and salts | Maintain optimal enzymatic environment | pH stability, ionic strength, chemical compatibility with reaction |
| Positive Controls | Known inhibitors, activators, or reference enzymes | Assay validation and performance monitoring | Potency, specificity, commercial availability, stability |
| Plate Formats | 96-, 384-, 1536-well microplates | Reaction vessels for screening | Volume requirements, evaporation control, compatibility with detectors |
Advanced Applications in Clinical Biomarker Validation
Enzymatic activity assays play increasingly important roles in the development and qualification of pharmacodynamic biomarkers for enzyme-targeting therapies. In the context of inborn errors of metabolism and other enzyme deficiency disorders, these assays support diagnosis, pharmacokinetic/pharmacodynamic modeling, and efficacy assessment for therapeutic modalities including enzyme replacement therapy, small molecule chaperones, and gene therapies [32].
The biomarker validation pipeline requires extensive collaboration across multiple clinical centers and substantial financial investment [36]. Enzymatic assays must demonstrate analytical validity with coefficient of variation typically less than 30% to achieve adequate diagnostic sensitivity in clinical studies [36]. For novel biomarker candidates, validation should incorporate both retrospective and prospective sample cohorts that recapitulate the general population in terms of disease prevalence and stage [36].
Regulatory qualification of enzyme biomarkers demands particularly rigorous evidence. According to analyses of EMA biomarker qualification procedures, approximately 77% of challenges were linked to assay validity issues, with frequent problems including specificity, sensitivity, detection thresholds, and reproducibility [8]. These findings underscore the critical importance of robust enzymatic assay design and validation in successful biomarker development programs.
Robust enzymatic activity assays form the cornerstone of modern drug discovery and clinical biomarker development. Through careful attention to kinetic principles, appropriate technology selection, and rigorous validation protocols, researchers can generate high-quality data that reliably supports therapeutic development decisions. As precision medicine advances, enzymatic profiling will continue to provide essential functional data complementing genomic and proteomic analyses, particularly for the growing number of therapies targeting specific enzyme pathways. The ongoing evolution of detection technologies and validation standards will further enhance our ability to quantify enzyme activity in clinically relevant contexts, ultimately accelerating the development of novel biomarkers and targeted therapeutics.
References are available from the original sources cited throughout this guide.
The clinical validation of novel enzyme biomarkers hinges on the critical first step of selecting the appropriate biological specimen. This guide provides an objective comparison of serum, plasma, and alternative liquid biopsy sources, equipping researchers with the data and methodologies needed to navigate this complex landscape.
Comparative Analysis of Specimen Types
The table below summarizes the key characteristics, advantages, and limitations of various specimens used in liquid biopsy, based on current research and clinical applications.
Table 1: Comparison of Liquid Biopsy Specimen Types
| Specimen Type | Key Analytes | Primary Applications & Advantages | Major Limitations & Challenges |
|---|---|---|---|
| Plasma/Serum | ctDNA, CTCs, EVs, proteins (e.g., IFN-γ, CTLA-4) [38] [39] [40] | - Gold standard for most liquid biopsy applications [39].- Comprehensive snapshot of tumor molecular landscape [41].- High sensitivity for MRD monitoring and prognosis [42] [40]. | - Invasive collection via venipuncture.- ctDNA can be vanishingly low in early-stage disease [43].- Background of normal cell-free DNA confounds analysis [43]. |
| Urine | cfDNA, cfRNA, proteins, metabolites [38] [44] | - Fully non-invasive collection [44].- Promising for urological and other cancers (e.g., bladder, cervical) [45] [44].- Suitable for large-scale screening. | - Lower analyte concentration for non-urologic cancers.- Requires highly sensitive detection technologies.- Less established for multi-cancer applications. |
| Cervicovaginal Fluid / Pap Smear | ctDNA (methylation markers), proteins [44] | - Direct proximity to gynecologic organs [44].- Can detect ovarian and endometrial cancers earlier than plasma [44].- Leverages existing screening infrastructure. | - Limited to gynecologic malignancies.- Patient acceptance and cultural barriers for collection. |
| Uterine Lavage | ctDNA, CTCs [44] | - Very high sensitivity for endometrial and ovarian cancers [44].- Directly samples the uterine cavity. | - Highly invasive procedure, similar to a tissue biopsy [44].- Not suitable for general screening or repeated monitoring. |
| Cerebrospinal Fluid (CSF) | ctDNA, EVs, cells [38] | - High diagnostic yield for central nervous system (CNS) tumors [38].- Reflects the tumor microenvironment of the CNS. | - Highly invasive collection via lumbar puncture.- Significant patient discomfort and risk. |
Experimental Protocols for Key Specimens
Plasma-Based Circulating Tumor DNA (ctDNA) Analysis
Plasma is the most widely validated specimen for ctDNA analysis. The following protocol details the steps for a tumor-informed, next-generation sequencing (NGS)-based MRD detection assay, as used in landmark studies like the VICTORI trial for colorectal cancer [42].
Table 2: Key Reagents and Kits for Plasma ctDNA Analysis
| Research Reagent / Kit | Function in Workflow | Example Use-Case |
|---|---|---|
| cfDNA BCT Tubes (e.g., Streck, PAXgene) [43] | Preserves blood cell integrity, prevents genomic DNA contamination during storage/transport. | Blood collection; enables sample stability for up to 7 days at room temperature [43]. |
| MagMAX Cell-Free DNA Isolation Kit [40] | Extracts and purifies cfDNA from plasma samples. | Isolating cfDNA from 5 mL of plasma for downstream quantification and analysis [40]. |
| Qubit dsDNA HS Assay Kit [40] | Fluorometric quantification of isolated double-stranded DNA. | Precisely measuring the concentration of extracted cfDNA prior to library preparation [40]. |
| NeXT Personal / AVENIO (MRD Assays) [42] [45] | Tumor-informed, ultra-deep sequencing for MRD detection. | Tracking ctDNA in post-surgical patients to predict recurrence; demonstrated 87% sensitivity for recurrence in the VICTORI study [42]. |
| Ella Automated Microfluidic System [40] | Automated, high-sensitivity immunoassay for protein biomarkers. | Quantifying serum levels of soluble biomarkers like IFN-γ, CTLA-4, and PD-L1 [40]. |
Diagram 1: Plasma ctDNA MRD Analysis Workflow. This diagram outlines the key steps from blood collection to final clinical reporting, highlighting critical stages where specialized reagents are used.
Urine-Based Biomarker Analysis for Cervical Cancer Screening
Urine-based assays represent a frontier in fully non-invasive screening. A large-scale clinical study launched in 2025 is evaluating a urine-based HPV DNA test for cervical cancer screening in 17,000 women [45]. The protocol involves:
- Sample Collection: First-void urine samples are self-collected by participants using standardized kits, enabling decentralized and comfortable sampling [45] [44].
- DNA Extraction and Purification: Centrifugation and commercial nucleic acid extraction kits are used to isolate cell-free DNA from urine.
- Target Analysis: The primary endpoint uses PCR or NGS to detect high-risk HPV DNA sequences. Secondary analyses may include methylation testing of specific gene panels (e.g., RASSF1A, BRCA1) to improve specificity and predictive value [45] [44].
Serum Soluble Biomarker Profiling via Automated Immunoassay
This protocol is used to quantify soluble proteins like immune checkpoints and cytokines, which have demonstrated prognostic value in patients treated with immunotherapy [40].
- Sample Collection and Dilution: Serum is separated from clotted blood. For analysis on platforms like the Ella system, samples are typically diluted 1:2 with a provided diluent [40].
- Automated Microfluidic Immunoassay: The diluted serum is loaded into a proprietary, pre-coated cartridge (e.g., a custom multiplex cartridge for sPD-L1, sLAG-3, sTIM-3, sCTLA-4, or a single-plex cartridge for IFN-γ) and inserted into the Ella device [40].
- Quantification and Analysis: The platform automatically runs the assay. Protein concentrations (pg/mL) are calculated using the manufacturer's calibrated standard curve and integrated software [40].
Performance Data and Clinical Validation
The diagnostic performance of a test is measured by its sensitivity (ability to correctly identify disease) and specificity (ability to correctly identify non-disease). The table below compults key performance metrics for different specimen and analyte combinations from recent studies.
Table 3: Diagnostic Performance of Liquid Biopsy Modalities Across Specimens
| Specimen | Analyte / Technology | Cancer Type | Reported Performance | Clinical Context |
|---|---|---|---|---|
| Plasma | ctDNA (MRD Assay) [42] | Colorectal Cancer | 87% sensitivity for recurrence; No relapse in ctDNA- patients [42] | Post-surgical monitoring (VICTORI study) |
| Plasma | EV Protein Signature [41] | Multiple (e.g., Pancreatic, Ovarian) | 71.2% sensitivity, 99.5% specificity [41] | Early-stage multi-cancer detection |
| Plasma | MCED Test (Methylation) [42] | Multiple Cancers | 59.7% overall sensitivity; 98.5% specificity [42] | Multi-cancer early detection (AACR 2025) |
| Urine | cfRNA (uRARE-seq) [42] | Bladder Cancer | 94% sensitivity (LOD95 = 0.05%) [42] | MRD monitoring |
| Cervicovaginal | ctDNA Methylation [44] | Ovarian Cancer | Up to 97.8% sensitivity for specific genes (e.g., OPCML) [44] | Early detection |
| Uterine Lavage | ctDNA [44] | Endometrial Cancer | >95% sensitivity for detection [44] | Early diagnosis |
Diagram 2: Specimen Choice Determines Clinical Utility. This diagram illustrates the logical relationship from the initial choice of specimen to the final clinical value of the test, emphasizing that pre-analytical factors are a key determinant of success.
The Scientist's Toolkit: Essential Research Reagents
Successful validation of enzyme biomarkers requires a suite of reliable reagents and platforms.
Table 4: Essential Research Reagent Solutions for Liquid Biopsy
| Category | Specific Product Examples | Critical Function |
|---|---|---|
| Blood Collection Tubes | Streck cfDNA BCT, Qiagen PAXgene Blood ccfDNA Tubes [43] | Stabilize nucleated blood cells to prevent release of wild-type genomic DNA during transport, ensuring ctDNA integrity. |
| Nucleic Acid Extraction | MagMAX Cell-Free DNA Isolation Kit, QIAamp Circulating Nucleic Acid Kit [40] | Isolate high-purity, short-fragment ctDNA/cfDNA from plasma, urine, or other body fluids. |
| DNA Quantification | Qubit dsDNA HS Assay Kit [40] | Provide highly accurate fluorometric quantification of low-concentration DNA samples for library preparation. |
| Ultra-Sensitive Detection | NeXT Personal (Personalis), AVENIO (Roche), Signatera (Natera) [42] [45] | Tumor-informed MRD assays capable of detecting ctDNA at parts-per-million (ppm) levels. |
| Protein Biomarker Analysis | Ella Automated Microfluidic System (Bio-Techne) [40] | Automate rapid, reproducible, and high-sensitivity multiplexed immunoassays for soluble serum proteins. |
The integration of biomarkers into clinical trial design represents a paradigm shift from the traditional one-size-fits-all approach toward precision medicine. Biomarkers, which are biological measurements that provide insights into disease mechanisms and therapeutic responses, are now fundamental tools for optimizing patient selection and enhancing trial efficiency. Clinical trials that fail to account for the molecular heterogeneity of diseases often require larger sample sizes, incur higher costs, and demonstrate diluted treatment effects, as a significant proportion of enrolled patients may be non-responders. In fact, without targeted enrichment strategies, the probability of efficacy for many approved drugs may be no better than a coin toss for individual patients [46].
Biomarker-driven strategies, particularly patient stratification and enrichment, address these challenges by ensuring that the right patients are matched with the right therapies based on their biological characteristics. Enrichment designs specifically aim to increase the proportion of likely responders in a trial, thereby improving the probability of detecting a treatment effect. This approach is supported by regulatory agencies like the U.S. Food and Drug Administration (FDA), which have issued guidance on enrichment strategies to advance precision medicine [46]. The following sections provide a comparative analysis of core biomarker-driven trial designs, complete with experimental data, methodological protocols, and visualizations to guide researchers in the clinical validation of novel enzyme biomarkers.
Core Biomarker-Driven Clinical Trial Designs
Biomarker-driven clinical trials can be implemented through several distinct design frameworks, each with specific applications, advantages, and operational considerations. The choice of design depends on the strength of evidence linking the biomarker to the treatment mechanism and the overarching goals of the clinical development program. The table below provides a detailed comparison of the four primary design archetypes.
Table 1: Comparison of Core Biomarker-Driven Clinical Trial Designs
| Trial Design | Key Principle | Primary Use Case | Example Biomarkers | Regulatory & Operational Considerations |
|---|---|---|---|---|
| Enrichment Design | Enrolls and randomizes only biomarker-positive participants [47]. | Predictive biomarkers with a strong mechanistic rationale for therapy; ideal for efficient signal detection [47] [46]. | EGFR mutations in NSCLC [47]. | - Can lead to narrower drug labels.- Requires robust, pre-planned assay validation and companion diagnostic strategy [47]. |
| Stratified Randomization | Enrolls all patients but randomizes them within pre-specified biomarker-positive and negative subgroups [47]. | Prognostic biomarkers; scenarios where both biomarker-high and biomarker-low patients are expected to benefit [47]. | PD-L1 expression in NSCLC [47]. | - Ensures balanced arms for unbiased efficacy comparison.- Requires understanding of whether the biomarker is prognostic, predictive, or both [47]. |
| All-Comers Design | Enrolls a broad population and assesses biomarker effect retrospectively via subgroup analysis [47]. | Earlier phase trials for hypothesis generation when the biomarker's role is not fully understood [47]. | Tumor Mutational Burden (TMB), circulating tumor DNA (ctDNA) [47]. | - Risk of diluted overall treatment effect if benefit is restricted to a subgroup.- Useful for generating hypotheses for future studies [47]. |
| Basket Trial Design | Enrolls patients with different cancer types but a shared biomarker into separate, non-comparable arms [47]. | Tumor-agnostic therapies with a strong predictive biomarker [47]. | BRAF V600 mutation across various solid tumors [47]. | - High operational efficiency from a single protocol.- Often employs Bayesian methods for statistical efficiency.- Naturally adaptable, allowing arms to be expanded or discontinued [47]. |
The strategic selection of a trial design is a critical determinant of success. Furthermore, adaptive enrichment designs offer dynamic flexibility. These are multi-stage designs that allow trial modifications based on interim biomarker data. For instance, if a biomarker-negative subgroup shows futility at an interim analysis, enrollment can be stopped for that subgroup, and resources can be focused on the promising biomarker-positive population [48]. This approach requires careful planning of interim analysis timing, futility boundaries, and sample size re-estimation [48].
Experimental Data and Performance Metrics
Quantitative Impact of Enrichment on Trial Efficiency
The strategic use of biomarkers for patient enrichment has a quantifiable and profound impact on clinical trial efficiency. A simulation of a typical Phase III trial demonstrates that without enrichment, a trial may need to enroll 2,000 patients to achieve statistical significance, with only 35% of patients in the intervention arm actually responding to the therapy. In contrast, employing a biomarker to enrich the trial population can dramatically reduce the required sample size while increasing the response rate within the intervention group [46].
Table 2: Impact of Biomarker-Based Enrichment on Clinical Trial Parameters
| Trial Scenario | Total Sample Size | Proportion of Responders in Intervention Group | Relative Trial Size Reduction |
|---|---|---|---|
| Unenriched Trial | 2,000 patients | 35% | Baseline |
| Moderately Enriched Trial (70% responders) | ~1,000 patients | 70% | 2x |
| Highly Enriched Trial (Perfect biomarker) | ~200 patients | ~100% | 10x |
This reduction in sample size translates directly into significant cost savings and faster trial timelines, accelerating patient access to effective therapies [46].
Experimental Biomarker Panel for Patient Stratification
Robust biomarker validation is supported by concrete experimental data. A recent study on critically ill patients provides a compelling example of using a multi-biomarker panel for predictive enrichment. The research identified that patients with simultaneous signatures of pyroptosis and ferroptosis had the lowest survival probability, and a specific biomarker profile could stratify these high-risk individuals for targeted interventions [49].
Table 3: Experimental Biomarker Panel for Stratifying Critically Ill Patients
| Biomarker Category | Specific Biomarkers | Association with Clinical Outcome | Measurement Technique |
|---|---|---|---|
| Pyroptosis-Related | IL-1Ra, IL-18, GDF15 | Significantly elevated in non-survivors; predicts mortality [49]. | Validated bead-based multiplex immune assays on a Luminex platform [49]. |
| Ferroptosis-Related | Malondialdehyde (MDA), Catalytic Iron (Fec) | Levels associated with severity of organ dysfunction and probability of death [49]. | N-methyl-2-phenylindole colorimetric assay for MDA; modified bleomycin assay for Fec [49]. |
| Inflammation & Other | IL-1α, IL-6, IL-10, TNF, CHI3L1 | Improved clinical outcome prediction when combined with pyroptosis/ferroptosis biomarkers [49]. | Multiplex immune assays; sandwich ELISA for CHI3L1 [49]. |
Methodologies for Biomarker Analysis and Validation
Detailed Experimental Protocol for Biomarker Validation
The clinical validation of novel enzyme biomarkers requires a rigorous, multi-stage process. The following protocol outlines the key steps from sample collection to data analysis, as exemplified by recent studies.
- Step 1: Sample Collection and Handling. Blood samples are collected from consented study participants. In longitudinal studies, samples are taken at specified time points (e.g., daily for the first week in an ICU setting) [49]. Standardized procedures for collection tubes, centrifugation, and plasma/serum separation are critical. Aliquots should be stored at -80°C until analysis to preserve biomarker integrity.
- Step 2: Biomarker Measurement with Advanced Assays.
- Multiplex Immunoassays: For cytokine biomarkers (e.g., IL-18, IL-1Ra, IL-6), use validated bead-based multiplex immunoassays (e.g., on a Luminex instrument) [49]. This allows for the simultaneous quantification of multiple analytes from a single, small-volume sample, enhancing efficiency and conserving precious patient material.
- Colorimetric Assays: For oxidative stress markers like malondialdehyde (MDA), a colorimetric assay using N-methyl-2-phenylindole can be employed. Briefly, the sample is mixed with the reagent to form a chromogen, and concentration is determined by comparison to a standard curve [49].
- Enzyme-Linked Immunosorbent Assay (ELISA): While traditional, ELISA remains a common tool. However, advanced platforms like Meso Scale Discovery (MSD) offer greater sensitivity and a wider dynamic range through electrochemiluminescence detection [8].
- Step 3: Data Integration and Clinical Correlation. Biomarker levels are log-transformed for statistical analysis. The measured concentrations are then correlated with clinical endpoints such as 30-day survival, Sequential Organ Failure Assessment (SOFA) scores, or the incidence of acute kidney injury (AKI) [49]. Unsupervised clustering techniques can identify distinct patient endotypes based on their biomarker profiles [49].
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting the appropriate tools and reagents is fundamental to generating reliable and reproducible biomarker data.
Table 4: Essential Research Reagents and Platforms for Biomarker Analysis
| Item / Solution | Function in Biomarker Research | Key Considerations |
|---|---|---|
| Luminex Multiplex Assays | Simultaneously quantifies multiple proteins (e.g., cytokines) from a single small-volume sample [49]. | Ideal for biomarker panel validation; requires specialized instrumentation and validated antibody beads. |
| Meso Scale Discovery (MSD) U-PLEX Platform | Allows custom design of multiplex biomarker panels using electrochemiluminescence detection [8]. | Offers higher sensitivity and a broader dynamic range than ELISA; more cost-effective per data point than running multiple ELISAs [8]. |
| LC-MS/MS (Liquid Chromatography-Tandem Mass Spectrometry) | Analyzes hundreds to thousands of proteins or small molecules in a single run; highly specific and sensitive [8]. | Superior for detecting low-abundance species and for applications where immunoassays lack specificity; requires significant expertise. |
| Colorimetric Assay Kits (e.g., for MDA) | Measures specific metabolic byproducts or enzyme activities through color change. | Relatively simple and accessible; performance depends on kit quality and specificity of the chemical reaction. |
| Validated Antibody Pairs (for ELISA) | The core component of an ELISA, providing the specificity to capture and detect the target antigen. | Antibody quality is paramount; cross-reactivity must be minimized to ensure assay specificity. |
Visualizing Biomarker Strategy and Experimental Workflow
Decision Pathway for Biomarker Trial Design Selection
The following diagram illustrates the logical decision-making process for selecting an appropriate biomarker-driven trial design based on the current understanding of the biomarker's role.
Biomarker Trial Design Decision Pathway
Workflow for Validating a Novel Enzyme Biomarker Panel
This flowchart outlines the core experimental workflow for the analytical and clinical validation of a novel enzyme biomarker panel, from initial sample processing to final data interpretation.
Biomarker Panel Validation Workflow
The integration of biomarkers through strategic patient stratification and enrichment is no longer a niche approach but a cornerstone of modern, efficient clinical development. As demonstrated by the quantitative data and experimental protocols, these strategies directly address the challenges of disease heterogeneity, leading to smaller, faster, and more informative trials. The successful execution of these strategies hinges on a foundation of robust biomarker validation using advanced, fit-for-purpose analytical methods. As the field evolves with innovations in AI, multi-omics, and liquid biopsies, the ability to precisely match patients with therapies will only deepen, solidifying the role of biomarkers in bringing effective, personalized medicines to patients faster.
The clinical validation of novel enzyme biomarkers represents a frontier in personalized medicine, enabling earlier disease detection, accurate prognosis, and precise monitoring of therapeutic response. Enzymes, with their central roles in cellular pathways and high measurability in biological fluids, offer a powerful window into pathological states. This guide objectively compares the performance and validation of emerging enzyme biomarkers across three key therapeutic areas—oncology, metabolic disorders, and neurology—providing researchers and drug development professionals with critical experimental data and methodological insights to advance diagnostic and therapeutic development.
Novel Enzymes in Oncology
MGMT Methylation in Glioblastoma
Background: Promoter hypermethylation of the MGMT (O6-methylguanine-DNA methyltransferase) gene is a critical biomarker in glioblastoma, associated with improved response to temozolomide chemotherapy. A novel double-probe quantitative MSP (dp_qMSP) assay was developed to address standardization challenges in MGMT methylation detection [50].
Experimental Protocol: The clinical validation study involved 100 FFPE (Formalin-Fixed Paraffin-Embedded) glioblastoma samples. Researchers performed both the novel dpqMSP and conventional MSP methods, establishing an optimal cutoff for methylated samples using quantitative data from dpqMSP. Kaplan-Meier curves and time-dependent ROC curves were employed to compare methodologies for predicting progression-free survival (PFS) and overall survival (OS) [50].
Performance Data:
Table 1: Performance Comparison of MGMT Methylation Detection Assays
| Assay Method | Sensitivity | Specificity | Area Under Curve (AUC) for PFS/OS Prediction | Key Advantages |
|---|---|---|---|---|
| dp_qMSP (Novel) | Comparable to conventional MSP | Comparable to conventional MSP | Increased AUC time-dependent vs. conventional MSP | Improved standardization, quantitative results, competitive sensitivity |
| Conventional MSP | Reference standard | Reference standard | Reference standard | Established methodology |
Conclusion: The dp_qMSP assay demonstrated comparable performance to conventional MSP in identifying patients with favorable prognosis, with the added benefit of improved standardization and quantitative output, making it suitable for routine clinical use [50].
CA-62 in Breast Cancer
Background: The CLIA-CA-62 assay detects a novel carcinoma-specific mesenchymal marker expressed on epithelial cell surfaces during epithelial-mesenchymal transition (EMT). This low-weight membrane transport N-glycoprotein is released into the bloodstream from early-stage tumor cells [51].
Experimental Protocol: A blind clinical study analyzed 196 breast cancer patients (85% with DCIS, Stage I, or IIA) and 73 healthy controls using both CLIA-CA-62 and CA 15-3 ELISA assays. Results were compared against histopathological findings and published imaging data [51].
Performance Data:
Table 2: Performance of CA-62 vs. Established Biomarkers in Early Breast Cancer Detection
| Detection Method | Overall Sensitivity | Specificity | DCIS Sensitivity | Stage I Sensitivity | Stage II Sensitivity |
|---|---|---|---|---|---|
| CLIA-CA-62 | 92% | 93% | 100% | 97% | 85% |
| CA 15-3 ELISA | 27-46% | 80% | Not specified | Not specified | Not specified |
| Mammography | 63-80% | 60% | Varies by density | Varies by density | Varies by density |
Conclusion: The CLIA-CA-62 assay demonstrated superior sensitivity for early-stage breast cancer detection compared to both CA 15-3 and mammography, particularly for DCIS and Stage I cancers. This suggests potential utility as a supplemental screening tool to improve early detection rates [51].
Novel Enzymes in Metabolic Disorders
Triglyceride-Glucose (TyG) Index in Prediabetes
Background: Cardiovascular disease (CVD) risk prediction in prediabetes remains challenging. Among 13 emerging metabolic health-related indicators, the triglyceride-glucose (TyG) index demonstrated the best predictive performance for CVD risk in patients with prediabetes [52].
Experimental Protocol: Researchers analyzed data from 7,477 eligible participants in the NHANES (1999-2020) database, randomly divided into development (70%) and validation (30%) cohorts. Receiver operating characteristic (ROC) curves assessed the predictive efficacy of 13 metabolic indicators. Multivariate logistic regression identified independent risk predictors for nomogram construction [52].
Performance Data:
Table 3: Predictive Performance of TyG Index and Derived Nomogram for CVD in Prediabetes
| Predictive Model | Area Under Curve (AUC) | Components | Clinical Utility |
|---|---|---|---|
| TyG Index Alone | 0.694 | Triglycerides, Fasting Glucose | Single-marker screening |
| Integrated Nomogram | >0.70 (C-index) | Age, Gender, Hypertension, TyG, SHR, NLR | Individualized CVD risk assessment |
Conclusion: The TyG index emerged as the most effective single predictor of CVD risk among prediabetic patients. When incorporated into a multifactorial nomogram with age, gender, hypertension, stress hyperglycemia ratio (SHR), and neutrophil-to-lymphocyte ratio (NLR), it provided robust, individualized risk prediction with C-indexes exceeding 0.70 [52].
Novel Enzymes in Neurological Disorders
Enzyme Targets in Alzheimer's Disease and Parkinson's Disease
Background: Enzymes play pivotal roles in the pathogenesis of neurological disorders, influencing neurotransmitter metabolism, protein aggregation, and neuroinflammation. Key enzymes including acetylcholinesterase (AChE), monoamine oxidase (MAO), beta-secretase (BACE1), and caspases represent promising therapeutic targets and biomarkers [53].
Experimental Protocol: Research in this field encompasses diverse methodologies, from preclinical studies examining enzyme inhibition to clinical trials of natural and synthetic enzyme-targeting compounds. Multi-omics approaches, including metabolomics and bioinformatics analysis, are employed to elucidate enzymatic pathways in neurological disorders [54].
Performance Data:
Table 4: Key Enzyme Targets in Neurological Disorders and Their Therapeutic Modulation
| Enzyme Target | Associated Disorder(s) | Pathological Role | Therapeutic Approach | Research Status |
|---|---|---|---|---|
| Acetylcholinesterase (AChE) | Alzheimer's Disease | Neurotransmitter regulation, amyloid plaque formation | AChE inhibitors (e.g., donepezil) | Clinically validated for symptom management |
| Monoamine Oxidase (MAO) | Parkinson's Disease | Dopamine metabolism, oxidative stress | MAO inhibitors (e.g., selegiline) | Clinically validated |
| Beta-Secretase (BACE1) | Alzheimer's Disease | Amyloid-β production | BACE1 inhibitors | Multiple clinical trial failures; challenges with blood-brain barrier penetration |
| Caspases | Alzheimer's Disease | Amyloid-β processing, tau cleavage, neuroinflammation | Caspase inhibitors | Preclinical and early clinical development |
Conclusion: Enzyme-targeting strategies show varying degrees of success in neurological disorders. While AChE and MAO inhibitors are established treatments, developing therapies for novel targets like BACE1 has proven challenging. Recent approaches focus on multi-target directed ligands (MTDLs) that simultaneously modulate multiple enzyme systems [53].
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents for Novel Enzyme Biomarker Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Assay Kits | CLIA-CA-62, dp_qMSP kit, ELISA-based phospho-tau kits | Quantitative measurement of specific enzyme activity or biomarker levels |
| Antibodies | Anti-CA-62, anti-phospho-tau (T181, T217), anti-MGMT | Detection and quantification of target enzymes in various sample types |
| Sample Types | FFPE tissue, serum, plasma, cerebrospinal fluid (CSF) | Source material for biomarker analysis, each with specific preparation protocols |
| Analytical Instruments | Chemiluminescence analyzers, PCR systems, flow cytometers | Enable precise quantification of enzyme activity and biomarker levels |
| Reference Materials | Certified reference standards for metabolites (e.g., triglycerides, glucose) | Calibration and quality control for accurate measurements |
Signaling Pathways and Experimental Workflows
Enzyme Roles in Alzheimer's Disease Pathology
Clinical Validation Workflow for Novel Enzyme Biomarkers
The clinical validation of novel enzyme biomarkers continues to transform diagnostic and therapeutic approaches across oncology, metabolic, and neurological disorders. The case studies presented demonstrate how quantitative, standardized assays for targets like MGMT in glioblastoma, CA-62 in breast cancer, and the TyG index in prediabetes offer improved sensitivity, specificity, and clinical utility over traditional methods. Despite challenges—particularly in neurological disorders where blood-brain barrier penetration and target specificity remain obstacles—the ongoing development of sophisticated detection technologies and multi-target approaches promises to further enhance personalized medicine. For researchers and drug development professionals, these advances underscore the importance of rigorous clinical validation and standardization in translating novel enzyme biomarkers from research tools to clinical practice.
Navigating Pitfalls and Enhancing Rigor in Validation Studies
In the pursuit of precision medicine, biomarkers have become indispensable tools for diagnosing diseases, predicting treatment responses, and monitoring therapeutic outcomes. However, the path from discovery to clinical implementation is remarkably inefficient. Research indicates that only about 0.1% of potentially clinically relevant cancer biomarkers described in literature progress to routine clinical use [8]. This staggering attrition rate represents a significant challenge for researchers, scientists, and drug development professionals working to translate novel enzyme biomarkers from bench to bedside.
The failure of biomarker candidates stems from a complex interplay of analytical, biological, and regulatory hurdles. For enzyme biomarkers specifically, challenges include maintaining enzymatic stability, accounting for pre-analytical variables, and demonstrating clinical utility beyond established markers [55] [2]. This guide examines the key failure points in the biomarker development pipeline and compares experimental approaches that can address these challenges, with a specific focus on novel enzyme biomarkers.
The Biomarker Attrition Landscape: Quantifying the Problem
The biomarker development pipeline involves multiple stages where candidates can fail, including discovery, analytical validation, clinical validation, and regulatory qualification [8]. Most failures occur not during initial discovery but during validation phases, where promising candidates face the harsh reality of clinical application.
Table 1: Biomarker Attrition Rates Across Development Stages
| Development Stage | Success Rate | Primary Failure Causes |
|---|---|---|
| Discovery & Initial Identification | 100% (Baseline) | N/A |
| Analytical Validation | ~10-15% | Lack of reproducibility, matrix effects, narrow dynamic range |
| Clinical Validation | ~1-2% | Poor correlation with clinical outcomes, insufficient specificity/sensitivity |
| Regulatory Qualification & Clinical Implementation | ~0.1% | Failure to demonstrate clinical utility, regulatory standards not met |
The financial implications of these failures are substantial. Developing a single ELISA for biomarker validation can cost up to $2 million and take over a year, yet still has a high failure rate [56]. For enzyme biomarkers specifically, additional challenges include enzyme stability, substrate specificity, and interference from complex biological matrices [55].
Comparative Analysis of Biomarker Validation Platforms
Choosing the appropriate analytical platform is critical for successful biomarker validation. The table below compares three primary technologies used in biomarker validation, with particular considerations for enzyme biomarkers.
Table 2: Platform Comparison for Biomarker Validation
| Platform | Sensitivity | Multiplexing Capability | Dynamic Range | Cost per Sample (4-plex) | Considerations for Enzyme Biomarkers |
|---|---|---|---|---|---|
| Traditional ELISA | Moderate | Low (Single-plex) | Narrow | ~$61.53 [8] | Suitable for established enzymes; limited for novel enzymes without validated antibodies |
| Meso Scale Discovery (MSD) | High (Up to 100x ELISA) [8] | Medium (U-PLEX platform) | Broad | ~$19.20 [8] | Better for detecting low-abundance enzymes; reduced matrix effects |
| LC-MS/MS | Very High | High | Broad | Variable | Ideal for enzyme activity profiling and substrate specificity studies |
Key Failure Points in Biomarker Development
Pre-Analytical Variables: The Silent Assassin
Pre-analytical factors represent one of the most significant yet frequently overlooked causes of biomarker failure. For enzyme biomarkers, these variables are particularly problematic as they can directly impact enzymatic activity measurements [57].
Critical Pre-Analytical Factors:
- Sample Collection Timing: Enzyme levels can fluctuate due to circadian rhythms and nutritional status [57]
- Sample Processing Delays: Enzymatic degradation occurs if processing is not immediate [57]
- Hemolysis: Releases intracellular enzymes and interferes with assays [57]
- Storage Conditions: Temperature variations affect enzyme stability [57]
- Anticoagulant Use: Different anticoagulants can variably impact enzyme activity [57]
For novel enzyme biomarkers, establishing standardized protocols that account for these variables is essential. Studies have shown that inconsistent handling can cause variations exceeding 30-40% in enzyme activity measurements, potentially invalidating clinical correlations [57].
Analytical Validation Challenges
Analytical validity requires demonstrating that an assay reliably measures the biomarker of interest. Common failure points include:
1. Specificity and Sensitivity Issues Many enzyme biomarkers fail to achieve sufficient specificity for their intended use. For example, while traditional enzyme biomarkers like PSA for prostate cancer and CA-125 for ovarian cancer have been widely used, they often disappoint due to limitations in specificity, resulting in false positives and unnecessary invasive procedures [58]. Novel enzyme biomarkers must demonstrate superior performance characteristics to replace or supplement these established markers.
2. Reproducibility Problems Inter-laboratory variability remains a significant challenge. A review of EMA biomarker qualification procedures found that 77% of biomarker challenges were linked to assay validity issues, including problems with specificity, sensitivity, detection thresholds, and reproducibility [8].
3. Dynamic Range Limitations Many traditional ELISA platforms have relatively narrow dynamic ranges compared to multiplexed immunoassays, making them unsuitable for biomarkers with wide physiological and pathological concentration ranges [8].
Clinical Validation Hurdles
Clinical validity requires demonstrating that a biomarker consistently correlates with specific clinical endpoints. Key failure points include:
1. Lack of Correlation with Clinical Outcomes Many biomarkers show promise in initial discovery cohorts but fail to correlate with clinical outcomes in larger, more diverse populations. This is particularly true for enzyme biomarkers where activity may not directly correspond to disease severity or progression [2].
2. Inadequate Population Diversity Enzyme levels can vary significantly based on age, sex, and ethnicity. For example, metabolomic studies have found sex differences where males exhibit higher levels of certain amino acids, while women show higher levels of circulating fatty acids and phosphatidylcholines [57]. These differences are often age-dependent, making it imperative to account for demographic factors during validation.
3. Insufficient Lead Time Effective biomarkers should provide adequate lead time for early intervention. Many novel enzyme biomarkers fail because they appear too late in the disease process to enable meaningful clinical interventions [58].
Experimental Protocols for Robust Biomarker Validation
Protocol 1: Comprehensive Analytical Validation
Purpose: To establish analytical validity of a novel enzyme biomarker assay according to regulatory standards.
Methodology:
- Precision Studies: Perform within-run (n=20) and between-run (n=5 days) replicates at low, medium, and high concentrations
- Accuracy Assessment: Spike recovery experiments using known quantities of recombinant enzyme
- Linearity and Range: Serial dilutions to determine the assay's dynamic range
- Specificity Testing: Cross-reactivity studies with related enzymes and potential interfering substances
- Stability Studies: Evaluate enzyme stability under various storage conditions (-80°C, -20°C, 4°C) and freeze-thaw cycles
Acceptance Criteria: Total imprecision <15%; recovery 85-115%; demonstrated stability under claimed conditions [8]
Protocol 2: Clinical Validation in Diverse Populations
Purpose: To establish clinical validity across representative patient demographics.
Methodology:
- Cohort Selection: Recruit participants stratified by age, sex, and ethnicity
- Sample Collection: Implement standardized SOPs for sample collection, processing, and storage
- Blinded Analysis: Perform enzyme activity measurements blinded to clinical data
- Statistical Analysis: Determine optimal cutoff values using ROC analysis and assess correlation with clinical endpoints
- Multicenter Verification: Validate findings across at least three independent sites
Key Considerations: Account for comorbidities, medications, and lifestyle factors that may influence enzyme levels [57] [2]
Visualization: Biomarker Validation Workflow
Biomarker Validation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Enzyme Biomarker Validation
| Reagent Category | Specific Examples | Function in Biomarker Development |
|---|---|---|
| Reference Standards | Recombinant enzymes, synthetic substrates | Provide quantification standards and positive controls for assay development |
| Stabilization Cocktails | Protease inhibitors, antioxidant mixtures | Preserve enzyme activity during sample processing and storage |
| Detection Systems | Chromogenic/fluorogenic substrates, labeled antibodies | Enable measurement of enzyme concentration or activity |
| Interference Blockers | Heterophilic antibody blockers, albumin scavengers | Reduce matrix effects and improve assay specificity |
| Quality Control Materials | Pooled patient samples, commercial QC materials | Monitor assay performance across multiple runs |
Future Directions: Leveraging Emerging Technologies
Artificial Intelligence and Machine Learning
AI and ML are revolutionizing biomarker discovery and validation by mining complex datasets, identifying hidden patterns, and improving predictive accuracy [58] [59]. For enzyme biomarkers, AI-powered tools can predict substrate specificity, identify optimal assay conditions, and even suggest structural modifications to improve stability [13].
Multi-Omics Integration
The integration of genomics, proteomics, metabolomics, and transcriptomics provides a more comprehensive understanding of disease mechanisms and enables the identification of robust biomarker signatures [58] [59]. For enzyme biomarkers, this approach can reveal regulatory networks and functional pathways that enhance clinical interpretation.
Liquid Biopsy Technologies
Advances in liquid biopsy technologies enable non-invasive monitoring of disease-associated enzymes through analysis of circulating tumor DNA (ctDNA), exosomes, and other blood-based biomarkers [58] [59]. These platforms facilitate real-time monitoring of treatment responses and disease progression.
The high attrition rate of biomarker candidates reflects the rigorous process required to establish analytical and clinical validity. For novel enzyme biomarkers, success requires addressing pre-analytical variables early, implementing robust validation protocols, and demonstrating clear clinical utility across diverse populations. By understanding common failure points and leveraging emerging technologies, researchers can improve the efficiency of biomarker development and bring more reliable tools to clinical practice.
The future of enzyme biomarker validation lies in standardized protocols, multiplexed assessment platforms, and artificial intelligence-driven optimization. As these technologies mature, they offer the promise of reducing the current attrition rate and accelerating the delivery of precision medicine tools to patients in need.
The clinical validation of novel enzyme biomarkers is a cornerstone of advancing precision medicine, enabling earlier disease diagnosis, accurate prognosis, and effective therapy monitoring. However, the path from discovery to clinical application is fraught with technical challenges. Specificity, sensitivity, reproducibility, and matrix effects represent critical hurdles that can determine the success or failure of a biomarker. Overcoming these challenges requires not only robust experimental design but also the selection of appropriate analytical technologies. This guide provides a objective comparison of current biomarker validation platforms, details essential methodologies to address key validation parameters, and offers visual workflows to assist researchers in navigating the complex process of enzyme biomarker development.
Technology Platforms for Biomarker Validation: A Comparative Analysis
Selecting the appropriate analytical platform is a foundational decision in biomarker validation. The choice involves balancing multiple factors, including sensitivity, multiplexing capability, and cost. While the enzyme-linked immunosorbent assay (ELISA) has long been the gold standard, advanced technologies now offer significant advantages for rigorous validation.
Table 1: Comparative Analysis of Biomarker Validation Platforms
| Technology | Dynamic Range | Sensitivity | Multiplexing Capability | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| ELISA | Relatively narrow [8] | High | Low (typically single-plex) | Gold standard; high specificity; robust [8] | Antibody-dependent; potentially time-consuming development [8] |
| Meso Scale Discovery (MSD) | Broad dynamic range [8] | Up to 100x more sensitive than ELISA [8] | High (e.g., U-PLEX platform) [8] | Low sample volume; reduced cost per data point [8] | Requires specialized instrumentation |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Broad | Surpasses ELISA in sensitivity [8] | Very High (100s-1000s of proteins) [8] | High specificity and precision; label-free detection | Complex operation; high initial cost |
| Multiplex Immunoassays | Broad | High (platform-dependent) | High (dozens of analytes) | High efficiency for biomarker panels; conserved sample [60] | Potential for cross-reactivity; data analysis complexity [60] |
The economic argument for advanced platforms is compelling. For instance, measuring a panel of four inflammatory biomarkers (IL-1β, IL-6, TNF-α, and IFN-γ) using individual ELISAs costs approximately $61.53 per sample, whereas using an MSD multiplex assay reduces the cost to $19.20 per sample, representing a savings of $42.33 per sample [8]. This demonstrates that transitioning to more advanced platforms can yield both operational and economic efficiency, especially when validating multi-analyte panels.
Key Experimental Protocols for Addressing Validation Challenges
A fit-for-purpose validation approach, tailored to the biomarker's intended clinical use, is essential. The following protocols are critical for establishing the robustness of a novel enzyme biomarker assay.
Protocol for Assessing Matrix Effects
Purpose: To evaluate whether components in the sample matrix (e.g., plasma, serum) interfere with the accurate detection and quantification of the target enzyme biomarker [61].
- Sample Preparation: Prepare a set of calibration standards in a surrogate matrix (e.g., buffer or stripped matrix). Spike the same amount of analyte into at least six different lots of the intended biological matrix (e.g., individual human plasma lots).
- Analysis: Analyze all prepared samples using the validated assay.
- Calculation and Interpretation: Calculate the mean measured concentration for the samples spiked into the surrogate matrix and the individual biological matrix lots. Determine the precision (%CV) and accuracy (%Bias) for each.
- Acceptance Criterion: The precision should typically be <15% CV, and accuracy should be within ±20% of the nominal concentration. A significant deviation in the biological matrix lots indicates a matrix effect [61].
- Orthogonal Confirmation: Where possible, confirm results using an orthogonal method based on a different principle (e.g., comparing ELISA results with LC-MS/MS) to rule out method-specific interferences [61].
Protocol for Determining Specificity and Selectivity
Purpose: To ensure the assay specifically measures the intended enzyme biomarker and is not cross-reactive with related isoforms, precursors, or clipped variants.
- Cross-Reactivity Test: Spike potentially interfering substances (e.g., pro-enzyme forms, closely related enzyme family members, common co-medications) at high concentrations into the sample matrix.
- Analysis: Measure the apparent concentration of the target biomarker in the spiked samples and compare it to a control sample.
- Interpretation: The measured response in the spiked sample should not significantly differ from the control. Immunoreactivity of variants exceeding 30% may be a concern for specificity [61].
Protocol for Establishing Sensitivity (Lower Limit of Quantification)
Purpose: To define the lowest amount of the enzyme biomarker that can be quantitatively measured with acceptable precision and accuracy.
- Preparation: Prepare and analyze a minimum of five replicates of samples spiked with the analyte at the proposed Lower Limit of Quantification (LLOQ) concentration.
- Analysis: Process and analyze the LLOQ samples alongside a calibration curve.
- Acceptance Criterion: The LLOQ is accepted if the inter-assay precision (%CV) is ≤20% and the accuracy is within ±20% of the nominal concentration [60].
Protocol for Ensuring Reproducibility
Purpose: To demonstrate that the assay produces consistent results within and across runs, days, operators, and laboratories.
- Experimental Design: Analyze quality control (QC) samples at low, medium, and high concentrations over multiple separate assay runs (at least three).
- Calculation: Calculate both the intra-assay (within a single run) and inter-assay (between different runs) coefficient of variation (%CV) for the QC samples [60].
- Acceptance Criterion: The inter-assay precision (%CV) should be ≤15% for the QC samples to demonstrate robust reproducibility [60].
Visualizing the Workflow for Biomarker Validation
The following diagrams outline the logical progression and key decision points in the biomarker validation journey.
Biomarker Validation Pathway
Matrix Effect Assessment
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful biomarker validation relies on a suite of high-quality reagents and materials. The following table details key components and their functions in a typical validation workflow.
Table 2: Essential Research Reagents and Materials for Biomarker Validation
| Reagent/Material | Function in Validation | Key Considerations |
|---|---|---|
| Validated Antibody Pairs | Capture and detection of the target enzyme biomarker in immunoassays (ELISA, MSD). | Specificity for the target epitope, low cross-reactivity, high affinity. |
| Recombinant Enzyme / Protein Standard | Serves as the reference material for generating calibration curves and determining assay sensitivity. | High purity, accurate concentration, and well-characterized activity. |
| Quality Control (QC) Samples | Pooled biological samples used to monitor inter- and intra-assay precision and reproducibility [60]. | Should be prepared at low, mid, and high concentrations and stored in single-use aliquots. |
| Matrix from Disease-Relevant Populations | Biological samples (e.g., serum, plasma) used to assess matrix effects and clinical validity [61]. | Sourced from well-characterized cohorts; requires ethical approval. |
| Multiplex Assay Panels | Pre-configured panels (e.g., MSD U-PLEX) for simultaneous validation of multiple biomarkers [8]. | Reduces sample volume requirements and cost per data point. |
| Signal Detection Reagents | Substrates and reagents that generate a measurable signal (e.g., chemiluminescent, electrochemical). | Compatibility with the detection platform and high signal-to-noise ratio. |
The rigorous clinical validation of novel enzyme biomarkers is a multifaceted endeavor. Success hinges on a critical understanding of the interplay between specificity, sensitivity, reproducibility, and matrix effects. As regulatory standards evolve, a "fit-for-purpose" approach, leveraging advanced technologies like MSD and LC-MS/MS, becomes increasingly important. By adhering to detailed experimental protocols, utilizing a robust toolkit of reagents, and systematically navigating the validation workflow, researchers can overcome these critical challenges. This rigorous process is essential for translating promising enzyme biomarkers from the research bench into reliable tools that can inform clinical decision-making and advance the field of precision medicine.
In the field of clinical validation for novel enzyme biomarkers, the integrity of research findings is paramount. Robust study design serves as the first and most critical line of defense against biases that can compromise data interpretation and clinical application. As precision medicine advances, the demand for validated biomarkers to inform clinical decision-making has never been greater [62]. The journey from biomarker discovery to clinical implementation is long and arduous, with statistical considerations in study design playing a pivotal role in determining success. This guide examines the fundamental methodologies of randomization, blinding, and power calculations, comparing their implementation across different study designs to mitigate bias and enhance the reliability of enzyme biomarker research.
Randomization Procedures in Clinical Trials
Randomization is the foundation of any clinical trial involving treatment comparison, serving to mitigate selection bias and promote similarity of treatment groups with respect to important known and unknown confounders [63]. In the context of enzyme biomarker validation, proper randomization ensures that observed associations reflect true biological relationships rather than systematic errors in participant allocation.
Comparison of Randomization Techniques
The table below summarizes the key randomization procedures, their applications, and their statistical properties relevant to biomarker studies.
Table 1: Comparison of Randomization Techniques in Clinical Research
| Randomization Type | Methodological Approach | Key Advantages | Limitations | Best Applications in Biomarker Research |
|---|---|---|---|---|
| Simple Randomization | Computer-generated random numbers, coin tossing, or random number tables [64] [63] | Maximum randomness and unpredictability; simple to implement [63] | Risk of substantial imbalance in group sizes, especially in small samples [64] [63] | Large trials with sample sizes >1000 where imbalance is minimal [63] |
| Block Randomization | Random assignment within small blocks (e.g., 4, 6, or 8 participants) to ensure equal group sizes [64] | Guarantees balance in participant numbers throughout recruitment period [64] | Potential for selection bias if block size is known and not varied [64] [63] | Long-term biomarker studies with extended recruitment; small to medium sample sizes [64] |
| Stratified Randomization | Creation of strata based on prognostic factors, then simple randomization within each stratum [64] | Controls for known confounding variables; ensures balance of key covariates [64] | Limited to known confounders; complexity increases with multiple stratification factors [64] | Biomarker studies where known clinical variables (e.g., disease stage, age) significantly impact outcomes [64] |
| Cluster Randomization | Randomization of groups rather than individuals [64] | Practical when individual randomization is not feasible; reduces contamination | Complex statistical analysis required; reduced statistical power [64] | Biomarker screening programs where geographical or organizational factors are relevant |
Experimental Protocol: Implementing Stratified Block Randomization
For robust validation of novel enzyme biomarkers, we recommend a stratified block randomization approach with the following detailed methodology:
- Identify Stratification Factors: Select 2-3 key prognostic variables known to influence the disease outcome or biomarker expression (e.g., disease stage, age categories, prior treatment history) [64].
- Generate Randomization Sequence: Using statistical software (R, SAS), create a computer-generated random allocation sequence with permuted blocks of varying sizes (e.g., 4 and 6) within each stratum [64] [63].
- Implement Allocation Concealment: Securely store the randomization sequence through a central independent system or sealed opaque envelopes to prevent foreknowledge of assignments [64].
- Execute Random Assignment: As each eligible participant is enrolled and their stratification factors recorded, assign them to the next available slot in the appropriate stratum block [64].
- Document Deviations: Maintain rigorous documentation of any protocol deviations or violations to enable intention-to-treat analysis.
This combined approach balances the covariate control benefits of stratification with the predictable group size balance of block randomization, while varying block sizes helps maintain allocation concealment [64] [63].
Blinding Methodologies in Biomarker Research
Blinding (masking) prevents conscious or unconscious influence on study results by keeping participants, investigators, and outcome assessors unaware of treatment assignments [64]. In enzyme biomarker studies, blinding is particularly crucial during outcome assessment and laboratory analysis to prevent measurement bias.
Levels of Blinding and Implementation Challenges
Table 2: Blinding Strategies for Biomarker Validation Studies
| Blinding Level | Methodological Approach | Effectiveness in Bias Reduction | Implementation Challenges in Biomarker Studies | Solutions and Alternatives |
|---|---|---|---|---|
| Open Label | No blinding of participants or researchers | None; highest risk of multiple biases | N/A | Use only when blinding is impossible; implement blinded endpoint adjudication committee |
| Single-Blind | Participants are unaware of their assignment group | Reduces participant-reported outcome bias and placebo effects | Investigators may consciously or unconsciously provide differential care | Combine with objective biomarker endpoints and centralized laboratory testing |
| Double-Blind | Both participants and investigating team are blinded | Reduces assessment and performance biases; gold standard for clinical trials [64] | Difficult when treatments have distinctive appearances or side effects | Use matched placebos; separate clinical care team from outcome assessors |
| Triple-Blind | Participants, investigators, and statisticians are all blinded | Prevents bias in analysis and outcome interpretation | Complex logistics and maintenance of blinding integrity | Implement data coding; maintain blinding until database lock and initial analysis |
Experimental Protocol: Implementing Blinding in Biomarker Assays
For laboratory analysis of enzyme biomarkers, implement the following blinding protocol to prevent analytical bias:
- Sample De-identification: Replace participant identifiers with coded labels that do not reveal group assignment, treatment sequence, or clinical outcomes.
- Batch Randomization: Process samples in randomized batches that mix intervention and control specimens to distribute assay variability equally across groups [62].
- Blinded Laboratory Personnel: Ensure laboratory technicians performing the assays are unaware of the clinical hypotheses and group assignments.
- Automated Analysis: Where possible, use automated instrumentation and predefined analytical protocols to minimize subjective interpretation.
- Blinded Data Transfer: Transfer de-identified results to statisticians who remain blinded to group codes until the analysis plan is finalized.
The fundamental principle is that individuals who generate biomarker data should be kept from knowing the clinical outcomes to prevent bias induced by unequal assessment of biomarker results [62].
Power Calculations and Sample Size Determination
Adequate statistical power is essential for detecting true effects of enzyme biomarkers while minimizing false positives and false negatives. Power analysis ensures studies have a high probability of detecting clinically meaningful effect sizes, optimizing resource allocation and ethical conduct of research.
Comparative Approaches to Power Calculation
Table 3: Power Calculation Methods for Biomarker Study Designs
| Study Design | Key Parameters for Power Calculation | Statistical Methods | Advantages | Limitations |
|---|---|---|---|---|
| Parallel-Group RCT | Effect size, alpha (Type I error), power (1-Type II error), allocation ratio [63] | Traditional sample size formulas (t-tests, chi-square) | Straightforward calculation; widely understood | Requires accurate estimation of effect size; may require large samples for biomarker subgroups |
| Crossover & N-of-1 Designs | Within-subject correlation, number of treatment periods, carryover effects [65] | Linear mixed effects models; time-series analysis [65] | Increased power with fewer subjects; each subject serves as their own control [65] | Susceptible to carryover effects; complex implementation [65] |
| Biomarker Predictive Studies | Prevalence of biomarker-positive subjects, interaction effect size | Interaction test power analysis; simulation studies | Specifically designed for biomarker-treatment interaction | Requires accurate biomarker prevalence estimates |
| ANCOVA with Covariate Adjustment | Correlation between outcome and covariates, among covariates themselves [66] | ANCOVA power formulas; blinded sample size recalculation [66] | Increased power through variance reduction; handles continuous and categorical covariates | Challenging parameter specification at design stage [66] |
Experimental Protocol: Power Calculation for Predictive Biomarker Validation
For validating a novel enzyme biomarker as predictive of treatment response, implement the following power calculation protocol:
- Define Primary Endpoint: Specify whether the biomarker is prognostic (main effect) or predictive (interaction effect) [62]. For predictive biomarkers, the key analysis tests the treatment-by-biomarker interaction in a statistical model [62].
- Estimate Key Parameters:
- Set α (Type I error rate) to 0.05 and power (1-β) to 0.80 or 0.90
- Determine clinically meaningful effect size (e.g., hazard ratio for survival outcomes, mean difference for continuous measures)
- Estimate biomarker prevalence in the target population
- For ANCOVA, estimate correlation between outcome and baseline covariates [66]
- Select Statistical Test: For predictive biomarkers, use interaction test power analysis rather than subgroup analysis [62].
- Calculate Sample Size: Use appropriate formula or statistical software (e.g., R, PASS, G*Power). For complex designs like aggregated N-of-1 trials, consider simulation-based power analysis [65].
- Account for Practical Considerations: Inflate sample size to accommodate expected dropout rates (typically 10-20%) and potential technical failures in biomarker assessment.
- Consider Adaptive Approaches: For studies with uncertainty in parameters, implement blinded sample size recalculation methods that allow adjustment based on interim variance estimates without unblinding treatment assignments [66].
Integrated Study Design Workflows
The following diagrams illustrate how randomization, blinding, and power considerations integrate into cohesive study designs for enzyme biomarker validation.
Clinical Validation Pathway for Novel Enzyme Biomarkers
Randomization and Blinding Integration
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Enzyme Biomarker Validation
| Reagent/Tool | Specific Function | Application in Bias Mitigation | Examples & Alternatives |
|---|---|---|---|
| Central Randomization System | Generates and conceals allocation sequences in real-time | Prevents selection bias; ensures allocation concealment [64] [63] | Interactive Web Response Systems (IWRS); sealed opaque envelopes |
| Matched Placebos | Identical appearance, taste, and administration to active treatment | Maintains blinding integrity; prevents performance bias [64] | Custom pharmaceutical manufacturing; over-encapsulation |
| Automated Laboratory Platforms | Standardized sample processing and analysis | Reduces technical variability and operator-dependent bias [8] | LC-MS/MS [8]; Meso Scale Discovery (MSD) [8]; ELISA |
| Blinded Data Management Systems | Secure database with access controls and audit trails | Maintains blinding until analysis complete; prevents data manipulation | REDCap; clinical trial management systems; customized databases |
| Statistical Analysis Software | Implementation of pre-specified analysis plans | Ensures analytical consistency; facilitates randomization-based tests [63] | R, SAS, Stata with specialized clinical trial packages |
The rigorous clinical validation of novel enzyme biomarkers demands meticulous attention to study design elements that mitigate bias. Through comparative analysis, we have demonstrated that no single approach to randomization, blinding, or power calculation is universally superior; rather, the optimal strategy depends on the specific research context, biomarker characteristics, and practical constraints. Stratified randomization procedures enhance prognostic balance, comprehensive blinding protocols safeguard against measurement bias, and appropriate power calculations ensure reliable detection of clinically meaningful effects. By integrating these methodologies into cohesive study workflows and leveraging appropriate research tools, scientists can enhance the validity and translational potential of enzyme biomarker research, ultimately contributing to more personalized and effective healthcare interventions.
The clinical validation of novel enzyme biomarkers represents a critical pathway toward advancing precision medicine. Within this landscape, the fit-for-purpose validation framework has emerged as the scientific standard, ensuring that biomarker assays provide reliable, actionable data while optimizing resource allocation. This approach is fundamentally grounded in the International Organisation for Standardisation definition of method validation: "the confirmation by examination and the provision of objective evidence that the particular requirements for a specific intended use are fulfilled" [67] [68]. Rather than applying uniform, rigid criteria to all biomarkers, the fit-for-purpose paradigm mandates that the stringency of validation be dictated by the biomarker's position along the spectrum from exploratory research tool to definitive clinical endpoint [67].
The driving principle behind this tailored approach is context-of-use (COU), which defines the specific role a biomarker will play in drug development or clinical decision-making [69]. As emphasized by workshop leaders in the field, "no context, no validated assay" [69]. This framework acknowledges that the evidence needed to validate a biomarker for early drug discovery differs substantially from the requirements for a biomarker supporting pivotal regulatory decisions or patient selection. A properly executed fit-for-purpose validation establishes a clear chain of evidence connecting the biomarker's biological rationale, analytical measurement capabilities, and intended clinical application [67] [68].
Classification of Biomarker Assays and Their Validation Requirements
Categorizing Biomarker Assay Technologies
The American Association of Pharmaceutical Scientists (AAPS) and the US Clinical Ligand Society have established a classification system that categorizes biomarker assays into five distinct classes based on their quantitative capabilities and reference standards [67] [68]. This classification provides the foundation for determining which validation parameters must be evaluated for each assay type. Definitive quantitative assays utilize fully characterized reference standards representative of the endogenous biomarker and calibration curves to determine absolute quantitative values for unknowns [67]. In contrast, relative quantitative assays employ reference standards that are not fully representative of the biomarker, while quasi-quantitative assays lack calibration standards but provide continuous numerical data based on sample characteristics [67]. Qualitative assays are categorized as either ordinal (using discrete scoring scales) or nominal (providing yes/no results) [67].
The selection of an appropriate assay category depends on multiple factors, including the biological characteristics of the biomarker, available reagents and reference materials, and the level of quantitative precision required for the intended application. This classification system enables researchers to focus validation efforts on the most critical performance parameters for their specific technology platform, avoiding unnecessary characterization while ensuring sufficient rigor for the intended use.
Validation Parameters Across Assay Categories
The validation requirements for each assay category vary significantly, reflecting their different technological characteristics and applications. The table below summarizes the core validation parameters recommended for each class of biomarker assay based on consensus positions from leading experts in the field [67]:
Table 1: Recommended Performance Parameters for Biomarker Assay Validation by Category
| Performance Characteristic | Definitive Quantitative | Relative Quantitative | Quasi-Quantitative | Qualitative |
|---|---|---|---|---|
| Accuracy | + | |||
| Trueness (Bias) | + | + | ||
| Precision | + | + | + | |
| Reproducibility | + | |||
| Sensitivity | + (LLOQ) | + (LLOQ) | + | + |
| Specificity | + | + | + | + |
| Dilution Linearity | + | + | ||
| Parallelism | + | + | ||
| Assay Range | + (LLOQ-ULOQ) | + (LLOQ-ULOQ) | + |
For definitive quantitative assays, parameters such as accuracy, precision, and sensitivity (measured as lower limit of quantitation, LLOQ) form the core of validation [67]. The total error approach, which combines systematic error (bias) and random error (intermediate precision), provides a comprehensive assessment of analytical performance [67]. Relative quantitative assays share many requirements with definitive quantitative methods but place greater emphasis on parameters such as parallelism, which evaluates whether diluted samples behave similarly to calibrators [67]. For quasi-quantitative and qualitative assays, validation focuses more heavily on precision, specificity, and sensitivity, with less emphasis on establishing absolute quantitative accuracy [68].
Implementing the Fit-for-Purpose Approach: A Phase-Based Framework
The Five Stages of Biomarker Method Validation
Biomarker method validation proceeds through discrete, iterative stages that systematically build evidence supporting the assay's fitness for its intended purpose. The following diagram illustrates this multi-stage validation workflow and the key activities at each phase:
Stage 1: Purpose Definition and Assay Selection represents the most critical phase, where the intended use and context of the biomarker are clearly defined [67] [68]. This foundational stage determines all subsequent validation activities and establishes the criteria for evaluating fitness-for-purpose. Stage 2: Method Development and Planning focuses on assembling appropriate reagents, writing the method validation plan, and finalizing assay classification [67]. During Stage 3: Experimental Performance Verification, the technical parameters identified in Stage 1 are evaluated through rigorous experimentation, culminating in the creation of standard operating procedures [67]. Stage 4: In-Study Validation assesses assay performance in the clinical context, identifying potential issues related to patient sampling, collection, storage, and stability [67]. Finally, Stage 5: Routine Use establishes quality control monitoring, proficiency testing, and batch-to-batch quality assurance processes [67]. This phased approach incorporates continuous improvement through iterative refinement, allowing the validation process to cycle back to earlier stages as new information emerges or requirements evolve.
Case Study: GLDH Qualification for Liver Injury Detection
The recent qualification of glutamate dehydrogenase (GLDH) as a biomarker for drug-induced liver injury (DILI) in patients with muscle disease exemplifies the successful application of fit-for-purpose validation principles [6]. This case study demonstrates how a tailored validation approach can address specific limitations of existing biomarkers and create novel clinical utilities. For decades, serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) served as standard biomarkers for liver injury detection. However, because both enzymes are present in muscle, elevated levels are difficult to interpret in patients with muscle diseases such as Duchenne muscular dystrophy, creating a significant challenge for drug safety assessment [6].
Researchers from the Critical Path Institute's Predictive Safety Testing Consortium identified GLDH as a promising alternative biomarker because it is expressed primarily in the liver, with only trace amounts found in muscle [6]. Unlike ALT and AST, GLDH levels are not affected by muscle damage, making it a more specific indicator of liver cell injury. The validation approach was specifically tailored to demonstrate that GLDH could reliably detect drug-induced liver injury in this particular patient population where conventional biomarkers were confounded by muscle-specific effects [6]. After more than a decade of development and validation work, the U.S. Food and Drug Administration (FDA) qualified GLDH in 2025 for use in clinical trials to detect liver injury in participants with muscle disease or suspected muscle degeneration [6]. This qualification enables drug developers to utilize GLDH alongside current liver safety tests such as total bilirubin and alkaline phosphatase to provide clearer, more reliable understanding of whether a drug is causing harm to the liver in these specific patient populations [6].
Experimental Design and Practical Implementation
Key Methodologies for Different Validation Parameters
The experimental protocols for fit-for-purpose validation vary based on the assay category and intended use, but several established methodologies provide robust assessment of critical validation parameters. For accuracy assessment in definitive quantitative assays, the SFSTP (Societe Francaise des Sciences et Techniques Pharmaceutiques) recommends constructing an accuracy profile that accounts for total error (bias and intermediate precision) using a pre-set acceptance limit defined by the user [67]. This approach typically involves running 3-5 different concentrations of calibration standards and 3 different concentrations of validation samples (representing high, medium, and low points on the calibration curve) in triplicate on 3 separate days [67]. The accuracy profile produces a β-expectation tolerance interval that visually displays the confidence interval (e.g., 95%) for future measurements, allowing researchers to determine what percentage of future values are likely to fall within pre-defined acceptance limits [67].
Precision evaluation typically includes multiple components: repeatability (intra-assay precision), intermediate precision (inter-assay, inter-analyst, inter-day variability), and reproducibility (inter-laboratory variation) [67]. For biomarker assays, precision is often evaluated at multiple concentrations spanning the assay range, with acceptance criteria typically set at ≤25% CV (≤30% at LLOQ) for exploratory applications and tighter criteria (≤15-20% CV) for more advanced applications [67]. Sensitivity assessment involves establishing the lower limit of detection (LLOD) and lower limit of quantitation (LLOQ) through serial dilution of analyte in the appropriate matrix, with LLOQ representing the lowest concentration that can be measured with acceptable precision and accuracy [67]. Specificity experiments evaluate potential interference from matrix components, related substances, or concomitant medications through spike-and-recovery studies using individual and combined potential interferents [67].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of fit-for-purpose validation requires careful selection of reagents, reference materials, and analytical tools. The following table details key research reagent solutions and their functions in biomarker validation studies:
Table 2: Essential Research Reagent Solutions for Biomarker Validation
| Reagent/Material | Function in Validation | Key Considerations |
|---|---|---|
| Reference Standards | Serve as calibrators for quantitative assays; establish measurement traceability | Fully characterized vs. partially characterized; commutability with endogenous biomarker [67] [69] |
| Quality Control (QC) Materials | Monitor assay performance during validation and routine use | Endogenous QCs preferred over recombinant materials for stability assessment [69] |
| Matrix Samples | Evaluate specificity, selectivity, and matrix effects | Appropriate selection of biological matrix (plasma, serum, tissue); consider individual vs. pooled sources [69] |
| Binding Reagents | Enable specific detection of biomarker (antibodies, aptamers, etc.) | Specificity, affinity, lot-to-lot consistency; critical for immunoassays [67] |
| Stability Samples | Assess biomarker stability under various storage and handling conditions | Evaluate freeze-thaw, short-term, long-term, and process stability [67] |
The selection of appropriate reference standards deserves particular attention in biomarker validation. Unlike drug assays where pure, well-characterized reference standards are typically available, biomarker assays often face challenges related to the lack of true reference standards that are identical to the endogenous biomarker [69]. This limitation necessitates careful consideration of how recombinant calibrators differ from endogenous forms and may require the use of endogenous quality controls instead of recombinant materials for stability determination and assay performance monitoring [69]. Similarly, the choice of matrix for validation studies should reflect the actual sample matrix to be used in clinical studies, with consideration of potential interferences and pre-analytical variables that might affect biomarker measurement [69].
Navigating Validation Challenges and Regulatory Considerations
Addressing Common Validation Challenges
Biomarker validation presents several significant challenges that require strategic approaches within the fit-for-purpose framework. Pre-analytical variability represents one of the most substantial challenges, as biomarker measurements can be influenced by numerous factors before samples ever reach the testing laboratory [69]. These variables include biological factors (diurnal variation, diet, exercise), sample collection procedures (anticoagulant use, tube type), processing conditions (centrifugation time and temperature), and storage conditions (freeze-thaw cycles, storage duration) [69]. Controllable pre-analytical variables should be addressed through standardized protocols, while uncontrollable variables (e.g., patient demographics, disease status) must be documented and considered during data interpretation [69].
The transition from preclinical to clinical biomarkers presents another major challenge, as many promising biomarkers identified in laboratory settings fail to demonstrate the same predictive power in human trials [70]. This translational gap stems from species differences, cell line artifacts, and the complexity of human disease progression [70]. Advanced model systems such as patient-derived organoids, humanized mouse models, and microfluidic organ-on-a-chip platforms can improve translational predictability by providing more physiologically relevant environments for biomarker discovery and validation [70]. Additionally, the integration of multi-omics approaches (genomics, transcriptomics, proteomics, metabolomics) provides a comprehensive view of disease mechanisms and biomarker interactions, enhancing clinical applicability [70].
Regulatory Landscape and Quality Considerations
The regulatory perspective on biomarker validation emphasizes that assays must produce "accurate, reliable, and robust data to support regulatory decision-making" [69]. While regulatory agencies have accepted the fit-for-purpose approach, expectations increase substantially when biomarker data support pivotal determinations of safety or effectiveness [69]. The FDA's Biomarker Qualification Program provides a pathway for formal regulatory endorsement of biomarkers for specific contexts of use, as demonstrated by the recent qualification of GLDH for detection of liver injury in patients with muscle disease [6].
Two distinct but complementary concepts govern biomarker validation: analytical validation and clinical validation [71]. Analytical validation provides proof that the biomarker assay is technically robust and reliably measures what it is supposed to measure [71]. This encompasses parameters such as accuracy, precision, analytical sensitivity, and specificity, typically assessed under Clinical Laboratory Improvement Amendments (CLIA) requirements in the United States [71]. Clinical validation, in contrast, demonstrates that the biomarker can fulfill its intended clinical purpose, establishing relationships between the biomarker measurement and clinical endpoints [71]. This requires application of the biomarker to independent patient populations distinct from those used in discovery and development to avoid overfitting and ensure generalizability [71].
Table 3: Comparison of Analytical vs. Clinical Validation Requirements
| Aspect | Analytical Validation | Clinical Validation |
|---|---|---|
| Primary Focus | Technical assay performance | Clinical utility and applicability |
| Key Parameters | Accuracy, precision, sensitivity, specificity | Sensitivity, specificity, positive/negative predictive value, hazard ratios |
| Study Design | Controlled experiments with reference materials | Independent clinical cohorts representing target population |
| Regulatory Framework | CLIA, GLP, GCP | FDA Biomarker Qualification Program, EMA qualification advice |
| Common Pitfalls | Inadequate characterization of reference materials, insufficient precision | Overfitting, use of non-representative patient populations, failure to blind |
The fit-for-purpose principle represents a pragmatic, scientifically rigorous framework for biomarker validation that aligns validation stringency with clinical application and decision-making context. By tailoring validation requirements to the specific intended use of biomarker data, this approach ensures sufficient evidentiary standards while optimizing resource allocation throughout the drug development pipeline. The classification of biomarker assays into definitive quantitative, relative quantitative, quasi-quantitative, and qualitative categories provides a structured foundation for determining appropriate validation parameters [67]. Implementation through a phased approach—from purpose definition through routine use with continuous improvement—creates a systematic pathway for establishing assay fitness [67]. As biomarker applications continue to expand across therapeutic areas, the fit-for-purpose framework offers the necessary flexibility and rigor to advance novel enzyme biomarkers from research tools to clinically valuable assets in precision medicine.
Leveraging Outsourcing and CRO Partnerships for Specialized Expertise and Cost Efficiency
The era of precision medicine is driving an unprecedented demand for robust biomarker validation in drug development. For researchers and scientists focused on the clinical validation of novel enzyme biomarkers, the landscape presents a significant challenge: balancing the need for advanced, specialized technologies with the practical constraints of time and budget. While traditional methods like ELISA have long been the gold standard, emerging advanced technologies such as liquid chromatography tandem mass spectrometry (LC-MS/MS) and Meso Scale Discovery (MSD) now offer superior precision, sensitivity, and efficiency [8]. The journey to qualifying biomarkers for clinical use is fraught with obstacles, leading to a remarkably low success rate—only about 0.1% of potentially clinically relevant cancer biomarkers described in literature progress to routine clinical use [8]. This stark statistic underscores the critical need for more rigorous validation approaches.
Concurrently, the global contract research organization (CRO) market, valued at approximately $82 billion in 2024 and projected to reach $139.42 billion by 2029, offers a strategic solution [72]. Pharmaceutical and biotechnology sponsors are increasingly turning to CRO partnerships to navigate the complex biomarker validation pipeline, which encompasses discovery, analytical validation, clinical validation, and regulatory qualification [8] [73]. This guide objectively compares the performance of different outsourcing models and analytical technologies, providing researchers with data-driven insights to optimize their biomarker validation strategies for both scientific rigor and cost efficiency.
Comparative Analysis of Biomarker Validation Technologies
The selection of an analytical platform is a foundational decision in biomarker research. The following comparison details the performance characteristics of established and emerging technologies.
Table 1: Comparative Analysis of Biomarker Validation Technologies
| Technology | Key Principle | Dynamic Range | Analytical Sensitivity | Key Advantages | Typical Cost per Sample (USD) |
|---|---|---|---|---|---|
| ELISA | Analog colorimetric or chemiluminescent detection in a microplate format. | Relatively narrow [8] | High (Established gold standard) | Versatility, robustness, high-throughput capability [8] | ~$61.53 (for 4-plex inflammatory panel) [8] |
| Meso Scale Discovery (MSD) | Electrochemiluminescence (ECL) detection on carbon electrode arrays. | Broader than ELISA [8] | Up to 100x greater than ELISA [8] | Superior sensitivity, multiplexing (e.g., U-PLEX), low sample volume [8] | ~$19.20 (for 4-plex inflammatory panel) [8] |
| LC-MS/MS | Physical separation of molecules (LC) followed by mass-based detection (MS/MS). | Very broad | Surpasses ELISA [8] | High specificity, ability to analyze hundreds/thousands of proteins, freedom from matrix effects [8] | Varies by panel complexity (Generally higher for discovery) |
| Simoa (Single Molecule Array) | Digital ELISA with single-molecule detection in femtoliter wells. | >4 logs [74] | Attomolar (single-molecule) level [74] | Exceptional sensitivity for low-abundance biomarkers, fully automated platforms available [74] | Varies by assay (Premium for ultra-sensitive detection) |
The data reveals a clear trade-off between the established utility of ELISA and the enhanced performance of newer platforms. For example, a direct cost analysis for a four-inflammatory biomarker panel (IL-1β, IL-6, TNF-α, and IFN-γ) shows that using MSD's multiplex assay ($19.20 per sample) provides a significant saving of $42.33 per sample compared to using individual ELISAs ($61.53 per sample) [8]. Furthermore, technologies like Simoa have enabled the validation of critical neurological biomarkers like plasma phospho-Tau 217 for Alzheimer's disease, achieving clinical sensitivity and specificity of >90% when using a two-cutoff approach, performance that aligns with recommendations for diagnostic use [74].
Detailed Experimental Protocols for Advanced Biomarker Assays
Adopting advanced methodologies requires an understanding of their operational workflows. Below are detailed protocols for two key technologies: the MSD immunoassay and the Simoa digital immunoassay.
Protocol: Meso Scale Discovery (MSD) Multiplex Immunoassay
The following workflow is adapted from the U-PLEX platform, which allows researchers to design custom biomarker panels [8].
- Step 1: Plate Preparation. A multi-array 96-well plate pre-coated with capture antibodies on integrated carbon electrodes is selected. The plate is washed with a PBS-Tween buffer to prepare the surface for assay incubation.
- Step 2: Sample and Standard Incubation. Calibrators, quality control samples, and test samples are pipetted into the assigned wells. The plate is then sealed and incubated with shaking for 2 hours at room temperature to allow biomarkers to bind to their specific capture antibodies.
- Step 3: Detection Antibody Incubation. After washing the plate to remove unbound material, a mixture of biotinylated detector antibodies is added to each well. The plate is sealed and incubated again for 1 hour with shaking. These antibodies bind to different epitopes of the captured biomarkers.
- Step 4: Signal Generation and Readout. Following another wash, a solution containing an MSD SULFO-TAG streptavidin conjugate is added, which binds to the biotinylated detector antibodies. After a final wash, an MSD Read Buffer is added to the plate. The instrument applies a voltage to the plate electrodes, inducing electrochemiluminescence from the SULFO-TAG labels. The light signal is measured, and the intensity is directly proportional to the amount of biomarker present in the sample.
Protocol: Simoa Digital Immunoassay for Plasma p-Tau 217
This protocol, validated for clinical use under CLIA standards, demonstrates the process for a high-sensitivity neurological biomarker [74].
- Step 1: Bead Capture and Incubation. Paramagnetic beads coated with an anti-p-Tau 217 capture antibody (e.g., Janssen PT3) are mixed with the plasma sample in a reaction cuvette. This mixture is incubated to allow the target biomarker to bind to the beads.
- Step 2: Detection and Labeling. The beads are washed and resuspended. A biotinylated detector antibody (e.g., Janssen HT43, specific for the N-terminal of tau) is added and incubated, forming a sandwich complex. After another wash, a streptavidin-β-galactosidase (SβG) conjugate is added, which binds to the biotinylated detector.
- Step 3: Single-Molecule Detection (Digital Analysis). The beads are washed a final time and resuspended in a resorufin β-D-galactopyranoside (RGP) substrate solution. The bead mixture is then loaded into a Simoa array disc containing 216,000 femtoliter-sized wells. The beads are sealed into the wells. If a bead is labeled with an enzyme, the RGP substrate is hydrolyzed to produce a fluorescent resorufin signal confined within the well. This "on-off" digital signal is imaged and counted by the HD-X analyzer.
- Step 4: Data Reduction. The concentration of p-Tau 217 in unknown samples is interpolated from a logistic 4-parameter standard curve. The percentage of beads associated with a signal (i.e., "on" wells) provides a digital measure of the analyte concentration, enabling attomolar sensitivity [74].
The Scientist's Toolkit: Key Research Reagent Solutions
The successful execution of advanced biomarker assays relies on a suite of critical reagents. The following table details essential components for the Simoa p-Tau 217 assay, which can serve as a model for other validation projects [74].
Table 2: Essential Research Reagents for a Digital Immunoassay (e.g., Simoa p-Tau 217)
| Reagent / Material | Composition / Type | Critical Function in the Assay |
|---|---|---|
| Capture Beads | Paramagnetic microbeads covalently coupled with a monoclonal anti-p-Tau 217 antibody. | Isolates and enriches the specific target biomarker (p-Tau 217) from the complex plasma matrix. |
| Biotinylated Detector Antibody | Monoclonal antibody (e.g., anti-tau HT43) conjugated to biotin. | Binds to a different epitope of the captured biomarker, enabling specific detection and signal amplification. |
| Enzyme Conjugate | Streptavidin-β-galactosidase (SβG). | Links the biotinylated detector to the enzymatic reaction; streptavidin binds biotin with high affinity. |
| Calibrators | Purified, HPLC-purified peptide construct of the target biomarker at known concentrations. | Creates the standard curve for interpolating biomarker concentration in unknown samples. |
| Sample Diluent | PBS-based buffer with heterophilic blockers, EDTA, and surfactant. | Preserves biomarker stability, minimizes non-specific binding, and reduces matrix interference. |
| Substrate | Resorufin β-D-galactopyranoside (RGP). | Enzyme substrate hydrolyzed by β-galactosidase to produce a fluorescent signal for detection. |
Navigating CRO Partnership Models for Biomarker Validation
Outsourcing biomarker validation to a CRO requires choosing an engagement model that aligns with the project's scope and the sponsor's internal resources. The industry is witnessing a shift away from traditional full-service models toward more hybrid strategies [75].
Table 3: Comparison of Clinical Research Organization (CRO) Partnership Models
| Partnership Model | Description | Best Suited For | Reported Sponsor Perceptions & Considerations |
|---|---|---|---|
| Full-Service CRO | A single CRO partner manages the entire clinical development process from start to finish. | Small to mid-sized biotechs, sponsors with complex multi-country trials, or those lacking internal infrastructure [76]. | Pros: End-to-end accountability, streamlined execution, global infrastructure [76]. Cons: Can be perceived as inflexible, with higher potential for change orders and less direct sponsor control [75] [77]. |
| Functional Service Provider (FSP) | The sponsor outsources specific clinical functions (e.g., data management, monitoring) to a CRO, while retaining overall trial leadership. | Sponsors with strong internal management teams who need to scale specific functions flexibly [76]. | Pros: Cost-effective for specific functions, allows sponsor to retain strategic control [75]. Cons: Requires significant sponsor oversight and coordination across multiple vendors [77]. |
| Hybrid Models | Blends in-house work, FSP, and full-service elements to create a tailored outsourcing strategy. | Sponsors seeking to balance control, cost, and access to specialized expertise; currently a growing trend [75] [77]. | Pros: Maximizes flexibility and access to best-in-class vendors for different needs [77]. Cons: Requires sophisticated vendor management and higher onboarding effort from the sponsor [75]. |
A 2025 industry assessment notes that sponsors using preferred provider (a type of full-service) models often reported spending significant time negotiating change orders, which introduces budget uncertainty [75]. Furthermore, a common perception among sponsors is that CRO teams, particularly at larger organizations, may be composed of a higher proportion of junior staff and can sometimes lack strong critical problem-solving skills, expecting instead to be told what to do [75]. This highlights the importance of diligent CRO selection and active partnership management, regardless of the chosen model.
Regulatory Considerations and the Future of Biomarker Validation
Engaging with regulatory agencies early in the biomarker validation process is critical for success. Both the FDA and EMA advocate for a tailored, fit-for-purpose approach to validation, meaning the level of validation should be aligned with the biomarker's intended use [8]. A review of the EMA biomarker qualification procedure revealed that a staggering 77% of challenges were linked to assay validity, with frequent issues concerning specificity, sensitivity, detection thresholds, and reproducibility [8]. This underscores the need for methodological precision and robust data.
Regulators are increasingly welcoming data generated from advanced technologies like MSD and LC-MS/MS due to their superior precision, sensitivity, and freedom from matrix effects [8]. A recent success story is the FDA's qualification of glutamate dehydrogenase (GLDH) as a safety biomarker for detecting drug-induced liver injury in clinical trials for patients with muscle disease. This achievement, led by C-Path's Predictive Safety Testing Consortium (PSTC), overcame the limitation of traditional markers like ALT and AST, which can be elevated due to muscle damage. The qualification of GLDH, a liver-specific enzyme, demonstrates how collaborative CRO partnerships can address long-standing clinical challenges and advance drug safety science [6].
Looking forward, several trends are poised to reshape biomarker validation in CRO partnerships:
- AI and Machine Learning: Integrating AI-driven algorithms for predictive analytics and automated data interpretation to accelerate biomarker discovery and validation [59].
- Multi-Omics Integration: Combining genomics, proteomics, and metabolomics data to achieve a holistic understanding of disease mechanisms and identify comprehensive biomarker signatures [59] [78].
- Liquid Biopsy Expansion: Advancing liquid biopsy technologies for non-invasive, real-time monitoring of disease progression and treatment response beyond oncology into other therapeutic areas [59].
- Decentralized Clinical Trials (DCT): Incorporating DCT elements as a standard offering to improve patient access, boost retention, and accelerate timelines [72] [76].
For researchers and drug development professionals engaged in the clinical validation of novel enzyme biomarkers, the strategic integration of advanced technologies and selective CRO partnerships is no longer a luxury but a necessity. The data clearly demonstrates that platforms like MSD, LC-MS/MS, and Simoa offer significant advantages in sensitivity, multiplexing capability, and cost-efficiency over traditional methods for complex panels. The choice of a CRO model—whether full-service, FSP, or a bespoke hybrid—should be a deliberate decision based on project scope, internal expertise, and the need for specialized capabilities.
The path to successful regulatory qualification is paved with rigorous, well-validated data. By leveraging the specialized expertise and technological infrastructure of CROs, sponsors can navigate the evolving regulatory landscape more effectively, de-risk their development programs, and ultimately accelerate the delivery of novel therapies to patients. As the field advances, embracing trends such as AI, multi-omics, and patient-centric trial designs through these partnerships will be key to unlocking the next generation of precision medicine.
Achieving Regulatory and Clinical Qualification Through Rigorous Evidence
In the field of novel enzyme biomarker research, the precise understanding and application of the terms "analytical validation" and "clinical qualification" are fundamental to developing robust, reliable, and regulatory-approved biomarkers. Despite being sometimes incorrectly used interchangeably, these processes represent distinct, critical stages in the biomarker development pipeline.
Analytical validation is the process of assessing the analytical performance of an assay—it confirms that the test method itself is reliable for accurately and consistently measuring the biomarker [79]. In contrast, clinical qualification (often termed "qualification" in regulatory contexts) is the evidentiary process of linking a biomarker, measured via a validated assay, to biological processes and clinical endpoints [79]. This guide will objectively compare these two concepts, providing clarity for researchers, scientists, and drug development professionals.
Defining the Concepts: Purpose and Scope
What is Analytical Validation?
Analytical validation establishes that the biomarker test method is scientifically sound and reproducible before its data can be meaningfully used in clinical studies [79]. It is an assessment of the assay's measurement performance characteristics, determining the range of conditions under which it will generate reproducible and accurate data [79]. The US Food and Drug Administration (FDA) and European Medicines Agency (EMA) provide clear protocols for this process, often guided by standards like ICH Q2(R1) for analytical procedures [80].
Core Objective: To ensure the assay reliably measures the biomarker of interest, focusing on the tool's performance rather than the biomarker's biological meaning.
What is Clinical Qualification?
Clinical qualification is the process of assessing the available evidence on the associations between the biomarker and disease states, including data showing the effects of interventions on both the biomarker and clinical outcomes [79]. It answers the question: Does the biomarker measurement meaningfully relate to the clinical or biological endpoint of interest?
Core Objective: To provide evidence that a biomarker is fit-for-purpose for a specific context of use, such as diagnosing a disease, predicting treatment response, or monitoring disease progression [8] [79]. Regulatory bodies like the FDA and EMA have introduced formal biomarker qualification processes to provide a stamp of approval for a biomarker's use in drug development [8].
The table below summarizes the key differences between analytical validation and clinical qualification.
Table 1: Core Differences Between Analytical Validation and Clinical Qualification
| Aspect | Analytical Validation | Clinical Qualification |
|---|---|---|
| Primary Focus | Technical performance of the assay or method [79] | Clinical/biological significance of the biomarker [79] |
| Fundamental Question | "Does the assay measure the biomarker accurately and reliably?" [79] | "Is the biomarker associated with the clinical endpoint or biological process?" [79] |
| Key Parameters | Accuracy, precision, specificity, sensitivity, limit of detection, robustness, linearity, and range [80] [81] | Strength of statistical association with clinical outcome, predictive value, and clinical utility [79] |
| Regulatory Guidance | ICH Q2(R1), CLIA [80] [74] | FDA Biomarker Qualification Evidentiary Framework, EMA Qualification of Novel Methodologies [8] |
| Stage in Pipeline | Earlier stage; prerequisite for qualification [79] | Later stage; relies on data from a validated assay [79] |
| Output | A reliable and reproducible testing method [80] | Evidence supporting a biomarker's interpretation for a specific use [79] |
The Interrelationship: A Sequential Workflow
Analytical validation and clinical qualification are distinct yet deeply interrelated steps in the biomarker evaluation framework. The process is sequential; a biomarker cannot be qualified for clinical use without an analytically validated assay to measure it [79]. The following diagram illustrates this workflow and its key components.
Figure 1: The biomarker evaluation process, showing the progression from analytical validation to clinical qualification and final utilization assessment.
Experimental Protocols and Performance Data
Protocol for Analytical Validation of a Novel Assay
Robust analytical validation follows established standards from organizations like the Clinical and Laboratory Standards Institute (CLSI). The protocol for validating a digital immunoassay for plasma phospho-Tau 217, as described by Quanterix, assesses the following parameters [74]:
- Precision: Repeatability (intra-assay) and intermediate precision (inter-assay, inter-operator, inter-instrument, inter-lot) are evaluated by testing multiple replicates of quality control samples across different conditions [74].
- Accuracy/Recovery: Determined by spiking a known quantity of the analyte (e.g., purified peptide) into a sample matrix and measuring the recovery percentage.
- Linearity: The assay is tested across its claimed measuring range by serially diluting a high-concentration sample and verifying that results fall along a linear curve [74].
- Limit of Detection (LOD) & Quantification (LOQ): LOD is determined by measuring blank samples and calculating the mean signal + 3 standard deviations. LOQ is the lowest concentration that can be measured with acceptable precision and accuracy (often ≤20% CV) [79].
- Specificity: Assessed by challenging the assay with potentially cross-reacting substances (e.g., other phosphorylated tau isoforms) to ensure no significant interference.
- Robustness: The assay's resilience to small, deliberate variations in operational parameters (e.g., incubation time, temperature) is tested.
Performance Benchmarks: Advanced vs. Traditional Methods
The choice of analytical platform directly impacts validation performance. Advanced technologies like Single Molecule Array (Simoa) and Meso Scale Discovery (MSD) often outperform traditional methods like ELISA, which is critical for detecting low-abundance enzyme biomarkers.
Table 2: Comparative Analytical Performance of Immunoassay Platforms
| Platform | Reported Sensitivity | Dynamic Range | Multiplexing Capability | Reported Cost per Sample (4-plex) |
|---|---|---|---|---|
| Traditional ELISA | Reference (Gold Standard) [8] | Narrow [8] | Single-plex | ~$61.53 [8] |
| Meso Scale Discovery (MSD) | Up to 100x greater than ELISA [8] | Broad [8] | High (e.g., U-PLEX platform) [8] | ~$19.20 [8] |
| LC-MS/MS | Superior to ELISA, suitable for low-abundance species [8] | N/A | High (100s-1000s of proteins) [8] | N/A |
| Simoa (Digital ELISA) | Attomolar level (single-molecule detection) [74] | Broad [74] | Limited | N/A |
Protocol for Clinical Qualification
Clinical qualification requires studies that rigorously link the biomarker to a clinical context. A study's eligibility criteria—defining who can participate—are paramount to achieving accurate results [82] [83]. The protocol for the Simoa p-Tau 217 assay provides a clear example [74]:
- Study Population: Enroll a well-defined cohort relevant to the intended use. For a diagnostic test, this includes symptomatic individuals and appropriate controls. The p-Tau 217 study included 873 symptomatic individuals from two independent clinical cohorts [74].
- Comparator Method: Use an established, gold-standard method to define the clinical truth. The p-Tau 217 assay used amyloid PET or CSF biomarkers as comparators [74].
- Statistical Analysis: Determine key metrics of clinical performance.
- Clinical Sensitivity: Ability to correctly identify diseased individuals (True Positive Rate).
- Clinical Specificity: Ability to correctly identify non-diseased individuals (True Negative Rate).
- Accuracy: Overall agreement with the comparator method.
- Cut-off Determination: Establish one or more cut-off values to optimize clinical decision-making. The p-Tau 217 assay used a 2-cutoff approach, creating an "intermediate zone" for which amyloid status was less certain, thereby maximizing confidence in the positive and negative predictions [74].
The Scientist's Toolkit: Essential Research Reagents and Materials
Success in developing and validating assays for enzyme biomarkers depends on high-quality, well-characterized reagents.
Table 3: Key Research Reagent Solutions for Biomarker Assay Development
| Reagent / Material | Function | Critical Considerations |
|---|---|---|
| Capture & Detector Antibodies | Bind specifically to the target enzyme biomarker to facilitate detection. | Specificity (e.g., monoclonal Jansen PT3 for p-Tau 217), affinity, and lot-to-lot consistency are paramount [74]. |
| Calibrators (Reference Standards) | Create a standard curve to convert assay signal into a quantitative concentration. | Should be pure, characterized (e.g., HPLC-purified, mass-spectrometry confirmed peptide), and gravimetrically prepared to ensure accuracy [74]. |
| Quality Control (QC) Samples | Monitor assay performance over time for precision and drift. | Should be matrix-matched (e.g., human plasma) and span low, mid, and high concentrations of the analyte. |
| Sample Diluent | Prepares the sample for analysis and minimizes non-specific background. | Often contains blockers (e.g., heterophilic blockers) to prevent interference and reagents to stabilize the analyte [74]. |
| Detection System (e.g., SβG Conjugate) | Generates a measurable signal proportional to the amount of captured biomarker. | Enzymatic activity (for SβG) and conjugation efficiency must be routinely monitored as part of quality control [74]. |
The journey from a discovered enzyme biomarker to a clinically useful tool is complex and rigorous. Analytical validation and clinical qualification are its two non-interchangeable pillars. The former ensures you have a precise and accurate ruler, while the latter proves that the measurements you take with that ruler have meaningful clinical implications. For researchers, a clear understanding of this distinction is not merely semantic—it is the foundation of a sound strategy for developing credible, regulatory-compliant, and clinically impactful biomarkers. Embracing advanced, validated analytical technologies and rigorous clinical qualification frameworks is essential for success in the era of precision medicine.
Biomarker qualification is a formal process through which drug developers can obtain regulatory endorsement for the use of a specific biomarker in drug development and regulatory decision-making. Both the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) have established structured pathways for biomarker qualification, though their approaches reflect distinct regulatory frameworks and procedural nuances. For researchers and drug development professionals, understanding these pathways is crucial for efficiently advancing novel enzyme biomarkers through the regulatory landscape. The FDA's Biomarker Qualification Program operates with a mission to "work with external stakeholders to develop biomarkers as drug development tools" with the goal of encouraging "efficiencies and innovation in drug development" [84]. Similarly, EMA's Committee for Medicinal Products for Human Use (CHMP) provides opinions "on the qualification of novel methodologies for medicine development" based on recommendations from its Scientific Advice Working Party [85].
FDA Biomarker Qualification Pathway
Regulatory Framework and Process
The FDA's biomarker qualification process is structured through the Biomarker Qualification Program (BQP) under the Center for Drug Evaluation and Research (CDER). The program's mission focuses on collaborating with external stakeholders to develop biomarkers as drug development tools that can advance public health by encouraging efficiencies and innovation in drug development [84]. The qualification process is guided by the framework established under the 21st Century Cures Act, which added new provisions to the Federal Food, Drug, and Cosmetic Act (FD&C Act) regarding biomarker qualification [86]. A key guidance document, "Biomarker Qualification: Evidentiary Framework," provides recommendations on general considerations for developing a biomarker for qualification, outlining that qualification represents a determination that "within the stated context of use, the biomarker can be relied on to have a specific interpretation and application in drug development and regulatory review" [86].
It is important to note that as of 2025, the FDA's qualification process is undergoing updates. As stated on their official website: "The process described in the guidance is no longer current and being rewritten. A new guidance will be published as soon as possible" [87]. This indicates an evolving regulatory landscape that researchers must monitor closely.
Submission and Review Elements
The FDA encourages early interaction and submission of biomarkers for qualification through a structured process. For current qualification projects and already qualified biomarkers, the FDA provides the CDER & CBER's DDT Qualification Project Search database [84]. The evidentiary standards required for qualification depend on the proposed Context of Use (COU), which precisely defines how the biomarker will be utilized in drug development and regulatory decision-making [86].
Table 1: Key Aspects of the FDA Biomarker Qualification Pathway
| Aspect | Description |
|---|---|
| Governing Regulation | 21st Century Cures Act [84] |
| Lead Office | CDER Biomarker Qualification Program (BQP) [84] |
| Key Guidance Document | Biomarker Qualification: Evidentiary Framework (2018, currently being updated) [87] [86] |
| Primary Focus | Qualification of biomarkers for specific Contexts of Use (COU) [86] |
| Public Consultation | Not explicitly mentioned in current guidelines |
| Current Status | Process is being revised; new guidance forthcoming [87] |
EMA Biomarker Qualification Pathway
Regulatory Framework and Process
The EMA approaches biomarker qualification through its system for "qualification of novel methodologies for medicine development." The CHMP issues qualification opinions based on recommendations from EMA's Scientific Advice Working Party [85]. This process leads to a CHMP qualification opinion or advice on the acceptability of a specific use of a method, which can apply to non-clinical or clinical studies, including the use of novel biomarkers [85]. A significant differentiator of the EMA process is its emphasis on public consultation: "Before finally adopting a qualification opinion, the CHMP makes its evaluation open for public consultation by the scientific community. This ensures that the CHMP shares information, as agreed with the applicant, and is open to scientific scrutiny and discussion" [85].
The EMA has also developed an "action plan for future-proofing qualification of novel methodologies" outlining steps the European medicines regulatory network plans to take in 2024 and 2025. This initiative aligns with the strategic goals of the European Medicines Agencies Network Strategy to 2025 and the EMA Regulatory Science Strategy to 2025, indicating a forward-looking approach to evolving regulatory science [85].
Submission and Review Elements
The EMA offers multiple levels of regulatory feedback:
- Qualification Opinions: Full opinions on the acceptability of a specific use of a method or biomarker [85]
- Qualification Advice: Guidance on protocols and methods intended to develop a novel method toward qualification [85]
- Letters of Support: Encouragement for promising methodologies that cannot yet be fully qualified, aimed at "encouraging data-sharing and facilitating studies aimed at eventual qualification" [85]
All CHMP qualification opinions are published, and letters of support may be published with sponsor consent [85].
Table 2: Key Aspects of the EMA Biomarker Qualification Pathway
| Aspect | Description |
|---|---|
| Governing Regulation | EMA Regulatory Framework for Novel Methodologies [85] |
| Lead Committee | CHMP with recommendations from Scientific Advice Working Party [85] |
| Key Document | Action plan for future-proofing qualification (2024-2025) [85] |
| Primary Focus | Qualification of novel methodologies for medicine development [85] |
| Public Consultation | Required before adopting qualification opinions [85] |
| Current Status | Active with published action plan for 2024-2025 [85] |
Comparative Analysis: Key Similarities and Differences
Strategic Approaches and Alignment
A comparative analysis reveals that while both agencies share the common goal of advancing robust biomarkers for drug development, their approaches reflect different strategic emphases. Both agencies require comprehensive data submissions to support biomarker qualification and emphasize the importance of context of use in evaluating biomarkers [88] [86]. However, the EMA places stronger emphasis on public consultation as an integral part of the qualification process [85], while the FDA's process is currently in a state of transition as it updates its guidance framework [87].
Recent comparative research examining FDA and EMA approaches in related areas highlights that "Harmonizing FDA and EMA guidelines is essential to streamline global clinical trials, reduce redundancies, and improve patient outcomes" [88]. This suggests that while differences exist, there is recognized value in alignment between the two major regulatory agencies.
Practical Implementation Considerations
From a researcher's perspective, several practical differences emerge:
- The EMA offers a more tiered approach to feedback, including qualification advice and letters of support for promising but not yet qualified biomarkers [85]
- The FDA provides a more centralized program through its BQP but is currently updating its process [87] [84]
- Both agencies encourage early engagement and consultation, though their specific procedural requirements differ [85] [86]
Table 3: Direct Comparison of FDA and EMA Biomarker Qualification Pathways
| Characteristic | FDA | EMA |
|---|---|---|
| Legal Foundation | 21st Century Cures Act [84] | EU Medicines Regulation [85] |
| Transparency | Qualified biomarkers listed in database [84] | Public consultation before opinion adoption [85] |
| Feedback Mechanisms | Qualification program interactions [84] | Qualification opinions, advice, and letters of support [85] |
| Status | Guidance being updated [87] | Active with published action plan for 2024-2025 [85] |
| Stated Goal | Advance public health through efficient drug development [84] | Quality opinions on novel methodologies [85] |
Experimental Validation Frameworks for Biomarker Qualification
Methodological Approaches for Clinical Validation
Successful biomarker qualification requires robust experimental validation demonstrating analytical and clinical validity within the proposed context of use. Methodologies commonly employed in biomarker development include:
- Transcriptomic Analysis: Utilizing datasets from repositories like the Gene Expression Omnibus (GEO) to identify differentially expressed genes [89]
- Weighted Gene Co-expression Network Analysis (WGCNA): Grouping genes with similar co-expression patterns into modules associated with disease states [89]
- Protein-Protein Interaction (PPI) Networks: Constructing interaction networks using databases like STRING to identify centrally connected hub genes [89]
- Machine Learning Techniques: Applying algorithms including LASSO, SVM-RFE, Boruta, and XGBoost to refine biomarker candidates [89]
- Experimental Validation: Conducting quantitative PCR, ELISA, or other laboratory methods to confirm biomarker expression differences [90] [89]
Experimental Workflow for Biomarker Validation
The following diagram illustrates a comprehensive experimental workflow for biomarker validation that incorporates regulatory considerations:
Research Reagent Solutions for Biomarker Validation
Table 4: Essential Research Reagents for Biomarker Validation Experiments
| Reagent/Resource | Function in Biomarker Validation | Example Application |
|---|---|---|
| Gene Expression Datasets | Provide transcriptomic data for initial biomarker discovery | GEO datasets (e.g., GSE63060, GSE63061) [89] |
| STRING Database | Constructs protein-protein interaction networks for identifying hub genes | PPI network analysis of candidate biomarkers [89] |
| CIBERSORT Algorithm | Estimates immune cell infiltration proportions from gene expression data | Assessing tumor microenvironment in cancer biomarkers [89] |
| ELISA Kits | Quantifies protein concentration of candidate biomarkers in patient samples | Measuring c-Myc protein in AD patient serum [89] |
| qPCR Reagents | Validates gene expression differences in candidate biomarkers | Experimental verification of biomarker genes [90] |
Strategic Recommendations for Researchers
Pathway Navigation and Submission Planning
For researchers planning biomarker qualification submissions, several strategic considerations can enhance the likelihood of success:
- Engage Early: Both agencies encourage early consultation to discuss proposed contexts of use and evidentiary requirements [85] [86]
- Define Precise Context of Use: Clearly articulate the specific drug development application for the biomarker, as qualification is granted for explicit contexts of use [86]
- Monitor Regulatory Updates: Particularly for FDA submissions, stay informed about the forthcoming updated guidance on biomarker qualification [87]
- Consider Parallel Advice: Explore opportunities for parallel scientific advice with both agencies to identify and address potential divergences early [88]
- Leverage Public Resources: Utilize existing qualified biomarkers and databases from both agencies to inform development strategies [85] [84]
Evidence Generation and Documentation
Building a comprehensive evidence package requires attention to several key areas:
- Generate Robust Analytical Validation Data: Demonstrate that the biomarker measurement is accurate, reproducible, and fit for purpose [90] [89]
- Include Diverse Populations: Ensure study populations reflect clinically relevant diversity, including race, ethnicity, and disease severity spectra [88]
- Utilize Multiple Methodological Approaches: Combine bioinformatics, machine learning, and experimental validation to build compelling evidence [89]
- Document Methodological Details: Thoroughly document protocols, including assay procedures, data processing methods, and statistical approaches [89]
- Address Potential Limitations: Proactively identify and address study limitations with additional analyses or data [88]
The evolving landscape of biomarker qualification reflects both agencies' commitment to advancing regulatory science while ensuring that qualified biomarkers provide reliable tools for drug development. By understanding the distinct pathways and requirements of both the FDA and EMA, researchers can strategically plan development programs that efficiently generate the evidence needed for successful biomarker qualification.
In the field of clinical validation of novel enzyme biomarkers, establishing analytical validity is a fundamental prerequisite for ensuring that research findings and clinical applications are built upon a reliable foundation. Analytical validity refers to the demonstration that a laboratory method or instrument is capable of accurately and reliably measuring the analyte of interest—in this context, enzyme biomarkers. For researchers, scientists, and drug development professionals, this process provides the critical assurance that their quantitative results truly reflect biological reality rather than methodological artifacts.
The journey from biomarker discovery to clinical implementation requires rigorous analytical validation to ensure that measurements are trustworthy across different laboratories, instruments, and timepoints. Without establishing these fundamental parameters, even the most promising biomarker candidates cannot progress toward regulatory approval or clinical adoption. This comprehensive guide examines the four cornerstone parameters of analytical validity—accuracy, precision, selectivity, and stability—within the specific context of enzyme biomarker research, providing both theoretical frameworks and practical experimental approaches for their determination.
Core Parameters of Analytical Validity
Accuracy and Precision: Distinction and Interrelationship
In analytical method validation, accuracy and precision represent two distinct but complementary aspects of measurement reliability. Accuracy refers to how close experimental measurements are to the true or accepted value, essentially measuring correctness [91] [92]. In the context of enzyme biomarkers, this translates to how well the measured enzyme concentration reflects the actual concentration present in the biological sample. Precision, meanwhile, refers to the consistency of measurements when repeated under identical conditions, measuring reproducibility [93] [94] [92].
The classical target analogy effectively illustrates this relationship: a tight cluster of arrows away from the bullseye represents precise but inaccurate measurements, while arrows scattered around the bullseye represent accurate but imprecise measurements, and a tight cluster in the bullseye represents both accurate and precise measurements [91] [92]. For enzyme biomarkers, this distinction is crucial—a method can consistently give the same wrong result (precise but inaccurate) or give correct results on average but with high variability (accurate but imprecise). Neither scenario is acceptable for clinical decision-making.
Statistical measurements for accuracy typically involve calculating percentage error: |(experimental value - true value)| / true value × 100% [91]. Measurements are generally considered accurate when the percentage error is less than 5%, though this threshold may vary based on clinical requirements [91]. Precision is typically quantified using measures of variation such as standard deviation or coefficient of variation across replicate measurements [93].
Selectivity and Specificity
Selectivity (often used interchangeably with specificity in analytical chemistry) refers to the ability of a method to unequivocally assess the analyte in the presence of other components that may be expected to be present in the sample matrix [93]. For enzyme biomarkers, these potential interferents include structurally similar enzymes, isozymes, degradation products, concomitant medications, or endogenous matrix components.
A highly selective method will generate a signal response exclusively attributable to the target enzyme biomarker, avoiding false positives from interferents [93]. This parameter is typically tested early in method validation because if the method cannot accurately distinguish the target analyte from other components, subsequent validation parameters become irrelevant [93]. In clinical applications, poor selectivity can lead to misdiagnosis or incorrect therapeutic monitoring, with potentially serious patient consequences.
Stability
Stability refers to the ability of the enzyme biomarker to maintain its chemical integrity and measurable activity under specified conditions and throughout the analytical process. Stability testing encompasses multiple scenarios relevant to the laboratory workflow: benchtop stability during processing, freeze-thaw stability through multiple cycles, short-term storage stability, and long-term stability in archival conditions [94].
For enzyme biomarkers, stability is particularly crucial as enzymes are inherently susceptible to denaturation, proteolytic degradation, or loss of catalytic function under suboptimal conditions. The complex matrices of biological samples (serum, plasma, tissue homogenates) can further impact stability through enzymatic degradation or binding interactions. Establishing stability profiles is therefore essential for defining appropriate sample handling, processing, and storage protocols that will preserve the analytical integrity of the enzyme biomarker throughout the pre-analytical phase.
Experimental Protocols for Establishing Analytical Validity
Determining Accuracy: Spike Recovery and Method Comparison
The most common technique for determining accuracy in enzyme biomarker studies is the spike recovery method, where a known amount of the purified enzyme biomarker is added (spiked) into the biological matrix, and the analysis is performed to determine how much of the added analyte can be recovered [94]. This experiment typically involves preparing samples with the target analyte added at 80%, 100%, and 120% of the expected concentration and performing the analysis in triplicate [94]. The percentage recovery is calculated as (measured concentration / theoretical concentration) × 100%.
For a comprehensive accuracy assessment, a comparison of methods experiment is performed by analyzing at least 40 different patient specimens by both the new test method and a validated comparative method [95]. The specimens should be carefully selected to cover the entire working range of the method and should represent the spectrum of diseases expected in routine application [95]. The experiment should extend over a minimum of 5 days to minimize systematic errors that might occur in a single run, with analysis of specimens ideally occurring within two hours of each other by both methods to preserve specimen integrity [95].
Table 1: Experimental Design for Accuracy Assessment via Method Comparison
| Parameter | Specification | Rationale |
|---|---|---|
| Sample Size | Minimum 40 patient specimens | Ensures statistical reliability [95] |
| Concentration Range | Cover entire working range | Assess accuracy across clinical decision points [95] |
| Timeframe | Minimum 5 days, ideally 20 days | Identifies between-run variability [95] |
| Analysis Timing | Within 2 hours for both methods | Prevents stability-related discrepancies [95] |
| Measurements | Duplicate recommended | Identifies sample mix-ups or transposition errors [95] |
Statistical analysis of comparison data typically involves linear regression for wide analytical ranges, providing estimates of systematic error at medically important decision concentrations [95]. The regression line (Y = a + bX) allows calculation of systematic error (SE) at critical decision levels (Xc) as SE = Yc - Xc, where Yc is the value from the regression line corresponding to Xc [95].
Assessing Precision: Replication Experiments
Precision assessment involves measuring replicates of the same sample under defined conditions and quantifying the variation between measurements. The International Conference on Harmonisation (ICH) guidelines categorize precision into three levels: repeatability (intra-assay precision), intermediate precision (inter-assay precision), and reproducibility (inter-laboratory precision) [94].
For enzyme biomarkers, a comprehensive precision study should include repeatability assessment using at least 9 determinations covering the specified range (e.g., 3 concentrations with 3 replicates each) [93]. This evaluates precision under the same operating conditions over a short interval. Intermediate precision should be assessed by having different analysts perform the tests on different days using different instruments, with the standard deviation of results calculated across these varying conditions.
Table 2: Experimental Design for Precision Assessment of Enzyme Biomarker Assays
| Precision Level | Experimental Approach | Acceptance Criteria |
|---|---|---|
| Repeatability | 9 determinations across assay range (3 concentrations × 3 replicates) under identical conditions [93] | CV < 5% for enzymatic assays |
| Intermediate Precision | Multiple analyses across different days, analysts, and equipment | CV < 10-15% depending on assay complexity |
| Reproducibility | Testing across multiple laboratories | Laboratory-specific criteria based on intended use |
The experimental workflow for precision assessment begins with preparing quality control samples at low, medium, and high concentrations across the analytical range. These samples are then analyzed according to the replication scheme, data on measured concentrations is collected, and statistical analysis including mean, standard deviation, and coefficient of variation is performed for each concentration level.
Establishing Selectivity: Interference Testing
Selectivity for enzyme biomarker assays is demonstrated by showing that the method can accurately measure the target enzyme in the presence of potential interferents present in the sample matrix. The experimental approach involves preparing samples containing the enzyme biomarker at a known concentration (typically near the lower and upper ends of the quantification range) and individually spiking them with potential interferents at clinically relevant concentrations.
Potential interferents to test for enzyme biomarkers include:
- Structurally similar enzymes and isozymes
- Co-administered medications (especially those likely to be used by the target patient population)
- Endogenous matrix components (lipids, bilirubin, hemoglobin for serum samples)
- Common metabolites that might cross-react with the detection system
The acceptance criterion for selectivity is typically that the mean measured concentration of the spiked sample should be within ±15% of the nominal concentration for each potential interferent tested. For enzyme biomarkers with known genetic variants or post-translational modifications, selectivity should also be demonstrated against these relevant variants.
Evaluating Stability: Protocol Design
Stability testing for enzyme biomarkers should evaluate stability under conditions that mirror actual sample handling, processing, and storage scenarios. The protocol should include:
- Bench-top stability: Samples kept at room temperature for specified timepoints (e.g., 0, 2, 4, 8, 24 hours)
- Freeze-thaw stability: Through multiple cycles (typically 3-5 cycles) at relevant storage temperatures
- Short-term storage stability: Refrigerated conditions if applicable
- Long-term storage stability: At the intended archival temperature (typically -70°C or -80°C for enzyme biomarkers)
- Processed sample stability: In autosampler conditions if applicable
For each stability experiment, quality control samples at low and high concentrations are analyzed in triplicate alongside freshly prepared standards. Stability is demonstrated when the mean concentration at each timepoint remains within ±15% of the initial concentration, with a precision of ≤15% CV.
Advanced Considerations in Enzyme Biomarker Validation
Integration with Clinical Validation
While establishing analytical validity is essential, it represents only the first step in the comprehensive clinical validation of novel enzyme biomarkers. The analytical methods must subsequently demonstrate clinical validity (ability to accurately predict the clinical condition of interest) and clinical utility (evidence that using the test improves patient outcomes) [7]. For enzyme biomarkers, this often involves establishing reference intervals in relevant populations, determining clinical decision limits, and demonstrating prognostic or predictive value in appropriately designed clinical studies.
Recent advances in machine learning and multi-omics integration are creating new opportunities and challenges in biomarker validation [7] [21]. These approaches can identify complex biomarker signatures that outperform single enzyme measurements but require even more rigorous validation to ensure analytical robustness across diverse populations and testing conditions [21]. The traditional validation parameters of accuracy, precision, selectivity, and stability remain fundamental, but their application may need extension to address these more complex biomarker models.
Regulatory and Quality Considerations
For enzyme biomarkers intended for clinical use or drug development support, analytical validation must align with regulatory expectations from agencies such as the FDA (U.S. Food and Drug Administration) and adhere to established guidelines from organizations like the International Conference on Harmonisation (ICH) [94]. Good Manufacturing Practice (GMP) regulations require "appropriate, scientifically valid methods" that are "accurate, precise, and specific for their intended purpose" [94].
The concept of "fitness for purpose" is central to regulatory acceptance—the degree to which data produced by a measurement process enables technically and administratively correct decisions for a stated purpose [94]. This means that the extent and stringency of analytical validation should be proportionate to the intended clinical application, with more impactful applications (such as definitive diagnosis or therapy selection) requiring more extensive validation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful analytical validation of enzyme biomarkers requires access to well-characterized reagents and reference materials. The following table outlines essential components of the research toolkit:
Table 3: Essential Research Reagent Solutions for Enzyme Biomarker Validation
| Reagent/Material | Function in Validation | Critical Quality Attributes |
|---|---|---|
| Certified Reference Material | Provides accuracy base with known concentration and purity [94] | Purity >95%, Certificate of Analysis with uncertainty measurement |
| Matrix-Matched Calibrators | Establish quantitative relationship between signal and concentration | Commutability with patient samples, stability, well-characterized matrix |
| Quality Control Materials | Monitor assay performance across precision experiments [95] | Three concentration levels (low, medium, high), defined acceptance ranges |
| Selective Inhibitors/Activators | Demonstrate assay specificity for target enzyme | Well-characterized mechanism, specificity for target enzyme |
| Stable Isotope-Labeled Analog | Internal standard for mass spectrometry-based methods | Identical analytical behavior, no isotopic interference |
| Antibody Reagents (if immunoassay-based) | Capture and detection in immunoassays | High affinity and specificity, minimal cross-reactivity |
| Enzyme-Stabilizing Buffers | Maintain enzyme integrity during stability assessments [94] | Compatible with assay system, preservatives to prevent degradation |
Establishing analytical validity through rigorous assessment of accuracy, precision, selectivity, and stability forms the essential foundation for the clinical validation of novel enzyme biomarkers. Without demonstrating these fundamental analytical performance characteristics, subsequent clinical correlations and utility claims lack credibility. The experimental approaches outlined in this guide provide a framework for generating robust evidence of analytical validity, while the recognition of advanced considerations highlights the evolving complexity of biomarker validation in the era of multi-omics and computational approaches.
For researchers and drug development professionals, investment in comprehensive analytical validation ultimately accelerates the translation of promising enzyme biomarkers from discovery to clinical application, ensuring that these important tools for precision medicine deliver on their diagnostic, prognostic, and predictive potential. As the field advances, maintaining rigorous standards for analytical validity while adapting to new technological paradigms will be essential for realizing the full promise of enzyme biomarkers in personalized healthcare.
In the field of precision medicine, establishing clinical validity is a critical step in translating novel enzyme biomarkers from research discoveries into clinically useful tools. Clinical validity refers to the ability of a biomarker to reliably correlate with or predict specific clinical endpoints and outcomes [62]. For researchers and drug development professionals, this process requires rigorous statistical methodologies to demonstrate that a biomarker accurately reflects biological processes, pathogenic processes, or pharmacological responses to therapeutic interventions [62].
The journey from biomarker discovery to clinical implementation is fraught with challenges, with only approximately 0.1% of potentially clinically relevant cancer biomarkers progressing to routine clinical use [8]. This high attrition rate underscores the necessity of robust statistical validation frameworks. For novel enzyme biomarkers, this validation process must establish meaningful correlations with clinically relevant endpoints, whether for diagnostic, prognostic, predictive, or pharmacodynamic applications [96].
This guide examines the core statistical methodologies, experimental protocols, and analytical frameworks essential for demonstrating the clinical validity of novel enzyme biomarkers, providing researchers with practical tools for navigating this complex landscape.
Statistical Framework for Biomarker Validation
Key Statistical Metrics and Their Interpretation
The validation of biomarker clinical utility relies on a suite of statistical metrics, each providing distinct insights into biomarker performance. The table below summarizes these essential metrics and their clinical relevance.
Table 1: Essential Statistical Metrics for Biomarker Validation
| Metric | Calculation | Clinical Interpretation | Ideal Range |
|---|---|---|---|
| Sensitivity | True Positives / (True Positives + False Negatives) | Ability to correctly identify patients with the disease | >80% for most applications |
| Specificity | True Negatives / (True Negatives + False Positives) | Ability to correctly identify patients without the disease | >80% for most applications |
| Positive Predictive Value (PPV) | True Positives / (True Positives + False Positives) | Probability that a positive test result truly indicates disease | Varies with disease prevalence |
| Negative Predictive Value (NPV) | True Negatives / (True Negatives + False Negatives) | Probability that a negative test result truly indicates no disease | Varies with disease prevalence |
| Area Under Curve (AUC) | Area under ROC curve | Overall ability to distinguish between disease and non-disease | 0.9-1.0 (excellent); 0.8-0.9 (good) |
| Hazard Ratio (HR) | Ratio of hazard rates between groups | Magnitude of difference in time-to-event outcomes | >1.5 or <0.67 for clinical significance |
These metrics collectively provide a comprehensive picture of biomarker performance. However, researchers must select metrics based on the intended use of the biomarker, as different applications (e.g., screening vs. prognosis) prioritize different performance characteristics [62].
Distinguishing Prognostic and Predictive Biomarkers
A fundamental distinction in biomarker validation lies between prognostic and predictive biomarkers, each requiring different statistical approaches and clinical validation pathways.
Table 2: Comparison of Prognostic vs. Predictive Biomarkers
| Characteristic | Prognostic Biomarker | Predictive Biomarker |
|---|---|---|
| Definition | Provides information about overall disease outcome regardless of therapy | Informs about differential response to a specific therapy |
| Study Design | Can be identified in single-arm studies or cohort studies | Requires randomized controlled trial data |
| Statistical Test | Main effect test in statistical model | Interaction test between treatment and biomarker |
| Clinical Question | "What is the natural history of this disease?" | "Who will benefit from this specific treatment?" |
| Example | STK11 mutation in non-squamous NSCLC [62] | EGFR mutation status for gefitinib response in pulmonary adenocarcinoma [62] |
Proper classification is essential, as the evidence requirements and statistical methods differ significantly between these biomarker types. Predictive biomarker validation specifically requires demonstration of a significant interaction effect between the biomarker and treatment in a randomized setting [62] [96].
Experimental Design and Methodological Considerations
Addressing Common Statistical Challenges in Validation Studies
Biomarker validation studies face several methodological challenges that can compromise results if not properly addressed. The following table outlines common statistical concerns and recommended solutions.
Table 3: Statistical Challenges and Solutions in Biomarker Validation
| Challenge | Impact on Validation | Recommended Solutions |
|---|---|---|
| Within-Subject Correlation | Inflated type I error rates, spurious findings | Use mixed-effects linear models, account for dependent variance-covariance structure [97] |
| Multiplicity/Multiple Testing | Increased false discovery rates | Implement false discovery rate (FDR) control, Bonferroni correction, pre-specified analysis plans [97] |
| Selection Bias | Compromised generalizability of findings | Use randomization in specimen analysis, prospective cohort designs, consecutive patient sampling [62] |
| Batch Effects | Technical artifacts mistaken for biological signals | Randomize case and control specimens across testing batches, implement batch correction algorithms [62] |
| Matrix Effects | Interference with analytical technique by sample components | Use sample clean-up methods, optimize dilution factors, incorporate internal standards [98] |
These challenges necessitate careful planning and statistical expertise throughout the validation process. Pre-specified statistical analysis plans are particularly crucial for avoiding data dredging and ensuring robust, reproducible findings [97] [96].
Analytical Platforms for Biomarker Validation
Selecting appropriate analytical platforms is crucial for generating reliable biomarker data. The field has moved beyond traditional ELISA methods toward more advanced multiplexed platforms that offer enhanced performance characteristics.
Table 4: Comparison of Biomarker Analytical Platforms
| Platform | Throughput | Dynamic Range | Multiplexing Capacity | Relative Cost |
|---|---|---|---|---|
| Traditional ELISA | Medium | Narrow (10²-10³) | Single-plex | Low (per analyte) |
| Multiplex Bead Arrays | High | Wide (10³-10⁴) | Medium (10-50 plex) | Medium |
| Meso Scale Discovery (MSD) | High | Very Wide (10³-10⁵) | Medium (10-25 plex) | Medium |
| LC-MS/MS | Medium | Wide (10³-10⁴) | High (100-1000+ plex) | High |
| Surface Plasmon Resonance | Low | Medium | Low to Medium | High |
Advanced platforms like MSD offer significant advantages, including up to 100 times greater sensitivity than traditional ELISA and broader dynamic range, enabling detection of lower abundance proteins [8]. For novel enzyme biomarkers, which may be present in low concentrations, this enhanced sensitivity can be critical for establishing meaningful clinical correlations.
Experimental Workflows for Clinical Validation
Integrated Validation Pathway for Novel Enzyme Biomarkers
The following diagram illustrates the comprehensive workflow for establishing the clinical validity of novel enzyme biomarkers, from initial measurement to clinical correlation:
This workflow emphasizes the systematic progression from analytical validation to clinical correlation, with each stage requiring specific statistical approaches and quality controls.
Detailed Experimental Protocol for Enzyme Biomarker Validation
For researchers designing validation studies, the following protocol provides a framework for generating statistically robust evidence of clinical validity:
Phase 1: Specimen Collection and Processing
- Collect specimens (serum, plasma, tissue) following standardized protocols to minimize pre-analytical variability
- Implement randomization of case and control specimens across testing batches to minimize batch effects [62]
- Aliquot and store specimens at -80°C with limited freeze-thaw cycles
- Document complete clinical metadata including patient demographics, disease stage, and prior treatments
Phase 2: Analytical Measurement
- Select appropriate analytical platform based on required sensitivity, specificity, and multiplexing needs
- For novel enzyme biomarkers, consider platforms like MSD or LC-MS/MS for enhanced sensitivity [8]
- Incorporate quality controls including standards, blanks, and replicates in each batch
- Determine enzyme activity or concentration using validated assays with established linear ranges
Phase 3: Statistical Analysis
- Pre-specify statistical analysis plan including primary endpoints and analysis methods [96]
- Calculate sensitivity, specificity, PPV, NPV using 2x2 contingency tables
- Generate ROC curves and calculate AUC with confidence intervals
- For prognostic biomarkers: Use Cox proportional hazards models for time-to-event endpoints
- For predictive biomarkers: Test treatment-by-biomarker interaction terms in statistical models [62]
- Account for multiple testing using FDR control when evaluating multiple biomarkers [97]
- Assess potential confounding by clinical variables using multivariate models
Phase 4: Clinical Correlation
- Correlate biomarker levels with relevant clinical endpoints (overall survival, progression-free survival, treatment response)
- Validate findings in independent cohort when possible
- Assess clinical utility using decision curve analysis or similar methods
This comprehensive protocol emphasizes methodological rigor at each stage to ensure statistically valid and clinically meaningful results.
Essential Research Reagent Solutions
Successful biomarker validation requires access to high-quality reagents and analytical tools. The following table outlines essential research solutions for enzyme biomarker validation studies.
Table 5: Essential Research Reagent Solutions for Biomarker Validation
| Reagent Category | Specific Examples | Primary Function | Key Considerations |
|---|---|---|---|
| Capture Molecules | Monoclonal antibodies, nanobodies, aptamers | Specific binding to target enzyme | Specificity, affinity, cross-reactivity potential [98] |
| Detection Systems | Electrochemiluminescence, fluorescence, SERS | Signal generation and amplification | Sensitivity, dynamic range, compatibility [99] |
| Reference Materials | Recombinant enzymes, calibrated standards | Assay calibration and quantification | Purity, stability, commutability [98] |
| Matrix Interference Controls | Normal serum, albumin-depleted serum | Assessing and minimizing matrix effects | Source, composition, reproducibility [98] |
| Signal Enhancement Reagents | Streptavidin-biotin complexes, enzymatic amplifiers | Enhancing detection sensitivity | Compatibility, background signal, linearity [100] |
Quality reagents are fundamental to generating reliable data. Particularly critical are well-characterized capture molecules with high specificity and minimal cross-reactivity, as these directly impact assay performance and the validity of subsequent clinical correlations [98].
Establishing the clinical validity of novel enzyme biomarkers through robust statistical correlations with clinical endpoints remains a challenging but essential endeavor in precision medicine. By implementing rigorous statistical methodologies, selecting appropriate analytical platforms, and following structured experimental protocols, researchers can generate the high-quality evidence needed to advance biomarker candidates toward clinical application. The frameworks presented in this guide provide a roadmap for demonstrating meaningful relationships between enzyme biomarkers and clinical outcomes, ultimately supporting the development of more targeted and effective therapeutic strategies.
As the field evolves, emerging technologies and statistical approaches will continue to enhance our ability to validate biomarkers with greater precision and clinical relevance, accelerating the translation of scientific discoveries into improved patient care.
The translation of novel enzyme biomarkers from research discoveries to clinically actionable diagnostic tools represents a critical bottleneck in precision medicine. Despite a wealth of promising candidates in scientific literature, only approximately 0.1% of potentially clinically relevant cancer biomarkers progress to routine clinical use [8]. This staggering attrition rate highlights the formidable challenge researchers face in proving clinical utility and impact on patient management. The evolving regulatory landscape, exemplified by the FDA's Biomarker Qualification Evidentiary Framework and European Medicines Agency's Regulatory Science Strategy to 2025, now demands more rigorous validation standards that extend far beyond analytical performance [8].
The enzyme markers market reflects this tension between promise and practical implementation, projecting robust growth to reach an estimated USD 25,500 million by 2025 with a CAGR of 12.5% through 2033 [11]. This growth is fueled by advancements in diagnostic technologies and increasing emphasis on early disease detection, yet remains constrained by validation challenges. Enzyme biomarkers offer unique advantages as biological catalysts that provide dynamic information about physiological and pathological processes, often enabling earlier disease detection than structural biomarkers alone [2]. Their activity-based measurement can reveal functional changes in health status, making them particularly valuable for monitoring therapeutic responses and disease progression.
This guide objectively compares current technologies, methodologies, and evidence requirements for demonstrating that novel enzyme biomarkers can reliably inform clinical decision-making and ultimately improve patient outcomes.
Comparative Analysis of Enzyme Biomarker Validation Platforms
Analytical Performance Benchmarks
Table 1: Comparison of Major Biomarker Analytical Platforms
| Platform | Sensitivity | Dynamic Range | Multiplexing Capacity | Throughput | Cost per Sample (Approx.) |
|---|---|---|---|---|---|
| Traditional ELISA | Moderate (ng-pg) | Narrow (~2 logs) | Single-plex | Moderate | $15-20 (singleplex) |
| Meso Scale Discovery (MSD) | High (10-100x ELISA) | Broad (>4 logs) | Medium (10-plex) | High | $19-25 (4-plex) |
| LC-MS/MS | High to Ultra-high | Broad (>5 logs) | High (100s) | Medium | $30-50 (varies widely) |
| Simoa Digital Immunoassay | Ultra-high (fg) | Broad (>4 logs) | Low to Medium | Medium | $40-60 (specialized) |
The performance characteristics of analytical platforms fundamentally determine the clinical applicability of enzyme biomarkers. Traditional ELISA, while considered the gold standard for decades, presents limitations including relatively narrow dynamic range and moderate sensitivity [8]. Advanced platforms like Meso Scale Discovery (MSD) leverage electrochemiluminescence detection to provide up to 100 times greater sensitivity than traditional ELISA, enabling detection of lower abundance proteins and a broader dynamic range essential for monitoring subtle biological changes [8].
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) offers exceptional specificity and the ability to analyze hundreds to thousands of proteins in a single run, making it particularly valuable for biomarker panels and complex disease states [8]. For ultra-sensitive detection requirements, single molecule array (Simoa) technology provides digital immunoassay capabilities that enable measurement of biomarkers at attomolar concentrations, as demonstrated in validated assays for neurological disorders like Alzheimer's disease [74].
The economic case for advanced multiplexed platforms strengthens as biomarker panels grow more complex. For example, measuring four inflammatory biomarkers (IL-1β, IL-6, TNF-α, and IFN-γ) using individual ELISAs costs approximately $61.53 per sample, while MSD's multiplex assay reduces this to $19.20 per sample - representing a 69% cost reduction while simultaneously conserving valuable sample volume [8].
Clinical Validation Performance Metrics
Table 2: Clinical Validation Metrics for Recently Validated Biomarkers
| Biomarker | Disease Context | Sensitivity | Specificity | AUC | Clinical Utility |
|---|---|---|---|---|---|
| Plasma p-Tau 217 (Simoa) | Alzheimer's Disease (Amyloid Pathology) | >90% | >90% | 0.942 | Rule-in/rule-out amyloid pathology [74] |
| Lyso-Gb1 | Gaucher Disease | 100% | 100% | N/A | Diagnosis and treatment monitoring [101] |
| Multi-marker Panel (Aβ42/40, ptau-217, APOE4) | Alzheimer's Disease | 91% | 91% | 0.942 | Identifying anti-amyloid therapy candidates [102] |
| NDUFA1 & COX7C | Obsessive-Compulsive Disorder | Significant downregulation | Significant downregulation | N/A | Potential diagnostic biomarkers [103] |
Recent successfully validated biomarkers demonstrate the performance thresholds necessary for clinical adoption. The Simoa p-Tau 217 assay for Alzheimer's disease exemplifies the rigorous standards now expected, achieving >90% sensitivity and specificity using a two-cutoff approach to maximize predictive values [74]. This performance enabled its recognition as the only blood-based biomarker recommended by the Alzheimer's Association Workgroup with accuracy comparable to FDA-cleared CSF biomarker tests [74].
For rare diseases, lysosomal storage disorder biomarkers like Lyso-Gb1 for Gaucher disease demonstrate exceptional diagnostic performance with 100% sensitivity and specificity, while also serving as monitoring tools for treatment response [101]. The integration of multiple biomarkers further enhances clinical utility, as evidenced by the combination of Aβ42/40, ptau-217, and APOE4 for Alzheimer's pathology detection, which achieved 91% sensitivity and specificity while reducing indeterminate results from 15% to 10% [102].
The emergence of mitochondrial-related biomarkers like NDUFA1 and COX7C for obsessive-compulsive disorder illustrates the expanding scope of enzyme biomarkers beyond traditional applications, though their clinical utility remains under investigation [103].
Experimental Protocols for Clinical Validation
Analytical Validation Protocol
Robust analytical validation forms the foundation for clinical credibility. The following protocol outlines critical validation parameters:
Precision and Reproducibility Testing:
- Perform within-run, between-run, and between-laboratory precision studies following CLSI EP05 guidelines
- Include at least 3 reagent lots, 2 instruments, and 5 operators over 5 days
- Test 3-5 levels of controls spanning the assay measuring range
- Acceptable precision: CV <15% (20% at LLOQ) for enzyme biomarkers
Linearity and Measuring Range:
- Prepare a series of dilutions from high-concentration patient samples
- Analyze in duplicate across the claimed measuring range
- Demonstrate recovery of 85-115% of expected values
- Determine LLOQ and ULOQ where precision meets acceptance criteria
Interference and Cross-Reactivity:
- Test common interferents (hemoglobin, bilirubin, lipids, rheumatoid factor)
- Evaluate cross-reactivity with structurally similar enzymes and isoforms
- Assess heterophilic antibody interference using blocking agents
Sample Stability:
- Evaluate freeze-thaw stability (3-5 cycles)
- Test short-term room temperature and refrigerated stability
- Determine long-term frozen storage stability at recommended temperatures
The Simoa p-Tau 217 validation exemplifies this approach, verifying performance across multiple instruments and reagent lots while establishing stability specifications under various storage conditions [74].
Clinical Validation Protocol
Clinical validation establishes the relationship between biomarker measurements and clinical endpoints:
Intended Use Population Definition:
- Clearly define the target population, disease stage, and clinical setting
- Include appropriate control groups (healthy, disease controls, mimics)
- Ensure demographic diversity reflecting intended use population
Reference Standard Comparison:
- Compare against clinically accepted reference standards (e.g., PET imaging, histopathology, clinical diagnosis)
- Blind biomarker testing to reference standard results
- Pre-specify statistical analysis plan including sensitivity, specificity, PPV, NPV
Longitudinal Monitoring Studies:
- Assess biomarker performance for treatment response monitoring
- Evaluate correlation with clinical improvement/deterioration
- Establish biologically significant change thresholds
The validation of plasma biomarkers for Alzheimer's disease demonstrates this protocol, comparing Aβ42/40 and ptau-217 against amyloid PET status in a diverse cohort while establishing cutoffs for clinical interpretation [102].
Visualization of Biomarker Development Workflows
Enzyme Biomarker Validation Pathway
Biomarker Development Pathway
Multi-Omics Integration Strategy
Multi-Omics Data Integration
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents for Enzyme Biomarker Validation
| Reagent Category | Specific Examples | Function in Validation | Key Considerations |
|---|---|---|---|
| Capture Antibodies | Anti-p-Tau 217 (Janssen PT3), Anti-tau (HT43) | Specific biomarker recognition | Epitope mapping, cross-reactivity testing, lot-to-lot consistency |
| Detection Systems | Biotin-Streptavidin-β-galactosidase, Electrochemiluminescence labels | Signal generation and amplification | Conjugation efficiency, stability, non-specific binding |
| Calibrators | Purified peptide constructs (HPLC-purified, mass-verified) | Standard curve generation | Purity verification, matrix matching, stability |
| Sample Diluents | PBS with heterophilic blockers, surfactants, protein stabilizers | Matrix effect minimization | Interference reduction, biomarker stability preservation |
| Quality Controls | Endogenous patient samples, spiked samples at multiple levels | Assay performance monitoring | Commutability with patient samples, concentration near medical decision points |
| Solid Phases | Paramagnetic microbeads (2.7μm carboxy), MSD plates | Immobilization support | Coupling efficiency, binding capacity, non-specific binding |
The selection and quality control of research reagents fundamentally determines the success of enzyme biomarker validation studies. High-affinity, well-characterized antibodies form the foundation of specific assays, as demonstrated by the anti-p-Tau 217 antibody (Janssen PT3) specific for an epitope spanning residues 210-220 with two phosphorylation sites (212 and 217) that enabled the development of a clinically validated Alzheimer's blood test [74].
Advanced detection systems like the biotin-streptavidin-β-galactosidase conjugate used in Simoa technology provide the signal amplification necessary for ultra-sensitive detection, while electrochemiluminescence labels in MSD platforms enable broad dynamic ranges [74] [8]. Critically, properly characterized calibrators - such as HPLC-purified peptide constructs with mass-based concentration determination - are essential for generating accurate standard curves and ensuring longitudinal assay consistency [74].
Sample diluents formulated with heterophilic blockers, EDTA, and surfactants play an often-underestimated role in minimizing matrix effects and interference, while commutable quality controls that behave like patient samples are indispensable for monitoring assay performance across reagent lots and instruments [74].
The validation of novel enzyme biomarkers for clinical utility represents a complex but navigable pathway requiring strategic integration of advanced analytical platforms, robust experimental protocols, and comprehensive clinical evidence generation. Success requires moving beyond traditional performance metrics to demonstrate tangible impacts on patient management decisions, therapeutic monitoring, and ultimately, clinical outcomes.
The emerging paradigm emphasizes multi-marker panels, high-throughput scalable technologies, and sophisticated data integration approaches that leverage machine learning and multi-omics strategies. As regulatory standards continue to evolve, researchers must adopt fit-for-purpose validation strategies that align with intended use claims while maintaining the flexibility to incorporate technological advancements.
By systematically addressing the analytical, clinical, and regulatory hurdles detailed in this guide, researchers can accelerate the translation of promising enzyme biomarkers from research discoveries to clinically impactful diagnostic tools that enhance patient care in the era of precision medicine.
Conclusion
The successful clinical validation of a novel enzyme biomarker is a multidisciplinary endeavor that demands scientific rigor, methodological precision, and strategic regulatory navigation. The journey from a promising discovery to a clinically useful tool hinges on a clear definition of clinical intent, the adoption of advanced and validated analytical methods, and a proactive approach to overcoming common pitfalls in specificity and reproducibility. As regulatory frameworks evolve, exemplified by the latest FDA guidance, and technologies like AI, multi-omics, and liquid biopsies mature, the future holds immense promise. By adhering to a structured validation roadmap, researchers can unlock the full potential of novel enzyme biomarkers, paving the way for more precise diagnostics, smarter clinical trials, and truly personalized therapeutic strategies that improve patient outcomes.
References
- 1. Biomarker definitions and their applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5813875/]
- 2. a systematic review of novel enzymes as biomarkers over the ... [https://jlpm.amegroups.org/article/view/8770/html]
- 3. Biomarkers as Biomedical Bioindicators: Approaches and ... [https://www.mdpi.com/1999-4923/15/6/1630]
- 4. Biomarkers as Biomedical Bioindicators: Approaches and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10303887/]
- 5. Diagnostic Enzymes Part 1: Enzyme Biomarkers | Blog [https://www.biosynth.com/blog/enzyme-biomarkers]
- 6. FDA Qualifies C-Path Biomarker GLDH to Detect Liver ... [https://c-path.org/fda-qualifies-c-path-biomarker-gldh-to-detect-liver-injury-in-clinical-trials/]
- 7. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 8. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 9. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 10. Novel biomarkers for diagnosis, prognosis, targeted therapy ... [https://biomarkerres.biomedcentral.com/articles/10.1186/2050-7771-1-1]
- 11. Enzyme Markers 2025-2033 Overview: Trends, Competitor ... [https://www.archivemarketresearch.com/reports/enzyme-markers-334280]
- 12. Enzyme Markers Market Report | Global Forecast From ... [https://dataintelo.com/report/global-enzyme-markers-market]
- 13. Enzyme specificity prediction using cross-attention graph ... [https://www.nature.com/articles/s41586-025-09697-2]
- 14. Recent progress in chemistry and bioactivity of novel ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425002466]
- 15. Novel enzyme found in gut bacteria could revolutionize ... [https://www.sciencedaily.com/releases/2025/03/250306122911.htm]
- 16. Computational scoring and experimental evaluation of ... [https://www.nature.com/articles/s41587-024-02214-2]
- 17. Robust enzyme discovery and engineering with deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11923063/]
- 18. Facilitating the Validation of Novel Protein Biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4586418/]
- 19. Analytical validation of novel cardiac biomarkers used in ... [https://www.sciencedirect.com/science/article/abs/pii/S0002870315001143]
- 20. Development and Clinical Validation of Blood-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507441/]
- 21. Machine Learning in Biomarker Discovery for Precision ... [https://esmed.org/machine-learning-in-biomarker-discovery-for-precision-medicine/]
- 22. Serum metabolic profiling enables diagnosis, prognosis ... [https://www.nature.com/articles/s41467-025-61163-9]
- 23. Enzyme Substrates Market Trends & Demand 2025 to 2035 [https://www.futuremarketinsights.com/reports/enzyme-substrates-market]
- 24. Comparison of biomarkers and laboratory results in unaffected ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452437/]
- 25. The advantages and the limitations of LC-MS/MS and Elisa ... [https://www.biotrial.com/bioanalysis-lc-ms-ms-vs-elisa/]
- 26. Precision-Driven Biomarker Validation: A Biotech ... [https://www.criver.com/eureka/precision-driven-biomarker-validation-biotech-perspective-part-i]
- 27. FDA Guidance for Industry on Bioanalytical Method ... [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 28. Comparison of Liquid Chromatography Mass Spectrometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7068296/]
- 29. ELISA Comparison [https://www.mesoscale.com/en/technical_resources/our_technology/our_immunoassays/elisa_comparison]
- 30. Meso Scale Discovery - MSD [https://pacificbiolabs.com/meso-scale-discovery-msd/]
- 31. Correlation between LC-MS/MS and ELISA methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536777/]
- 32. Best Practices for Development and Validation of ... [https://pubmed.ncbi.nlm.nih.gov/39179710/]
- 33. Enzyme Assays: The Foundation of Modern Drug Discovery [https://bellbrooklabs.com/enzyme-assays-and-drug-discovery/?srsltid=AfmBOopy-QXYO9duO1tzEB1w17a3Ao67m9yymOH-PBOjFzsS8BlYxm1D]
- 34. Enzyme Assay Analysis: What Are My Method Choices? [https://www.thermofisher.com/blog/analyteguru/enzyme-assay-analysis-what-are-my-method-choices/]
- 35. Basics of Enzymatic Assays for HTS - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK92007/]
- 36. Biomarker Validation - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/biomarker-validation]
- 37. Guide to Enzyme Unit Definitions and Assay Design [https://resources.biomol.com/biomol-blog/guide-to-enzyme-unit-definitions-and-assay-design]
- 38. Fostering the implementation of liquid biopsy in clinical practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC12100835/]
- 39. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 40. Identification of prognostic liquid biopsy biomarkers in patients ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06957-7]
- 41. In Search of Ideal Solutions for Cancer Diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550977/]
- 42. Cancer in a Drop: Liquid biopsy insights from AACR 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223554/]
- 43. Improvement of the sensitivity of circulating tumor DNA- ... [https://www.explorationpub.com/Journals/etat/Article/1002333]
- 44. Clinical utility of various liquid biopsy samples for the early ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1594100/full]
- 45. Liquid Biopsy | September Round-Up 2025 [https://www.decibio.com/insights/liquid-biopsy-september-round-up-2025]
- 46. Clinical Trial Enrichment Strategies | Biomarker-Driven ... [https://sapient.bio/resources/biomarker-driven-clinical-trial-enrichment/]
- 47. Biomarker-Driven Clinical Trials in Oncology [https://www.precisionformedicine.com/blog/biomarker-driven-clinical-trials-in-oncology-enrichment-stratification-all-comers-basket-when-to-use-what-and-why]
- 48. Optimality Considerations in Two-Stage Biomarker ... [https://pubmed.ncbi.nlm.nih.gov/41248629/]
- 49. Potential of biomarker-based enrichment strategies to ... [https://www.nature.com/articles/s41418-025-01545-0]
- 50. Clinical validation of a novel quantitative assay for the ... [https://pubmed.ncbi.nlm.nih.gov/33750464/]
- 51. Clinical validation of the novel CLIA-CA-62 assay efficacy ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1009863/full]
- 52. Development and validation of a novel metabolic health ... [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-025-02445-5]
- 53. Alleviation of Neurological Disorders by Targeting ... [https://www.mdpi.com/1422-0067/26/10/4707]
- 54. Novel therapeutic target and drug discovery for neurological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11903713/]
- 55. Enzymes as indispensable markers in disease diagnosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11216522/]
- 56. Biomarker discovery pipeline: 3 Critical Steps 2025 [https://lifebit.ai/blog/biomarker-discovery-pipeline/]
- 57. Challenges in the Metabolomics-Based Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11051909/]
- 58. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 59. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 60. analysing, interpreting, and reporting biomarker data in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389263/]
- 61. Evaluating the impact of matrix effects on biomarker assay ... [https://pubmed.ncbi.nlm.nih.gov/24830892/]
- 62. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 63. A roadmap to using randomization in clinical trials [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01303-z]
- 64. Selection of Control, Randomization, Blinding, and Allocation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6743387/]
- 65. Optimizing Aggregated N-Of-1 Trial Designs for Predictive ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2020.00013/full]
- 66. Blinded sample size recalculation in randomized controlled ... [https://arxiv.org/abs/2508.18815]
- 67. Fit-for-purpose biomarker method validation for application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2990602/]
- 68. Fit-for-purpose biomarker method validation in anticancer ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644610002606]
- 69. Best practices for the development and fit-for-purpose ... [https://aapsopen.springeropen.com/articles/10.1186/s41120-021-00050-1]
- 70. Preclinical vs. Clinical Biomarkers: Understanding Their ... [https://blog.crownbio.com/preclinical-vs-clinical-biomarkers-understanding-their-distinct-roles-in-drug-development]
- 71. An introductory guide to biomarkers, precision, ... [https://www.almacgroup.com/diagnostics/diagnostic-resource/an-introductory-guide-to-biomarkers-precision-personalised-and-stratified-medicine/]
- 72. Top 10 CROs to Watch in 2025 [https://www.proclinical.com/blogs/2025-3/top-10-cros-to-watch-in-2025]
- 73. Pharmaceutical Contract Research Services Market Report [https://www.globenewswire.com/news-release/2025/09/24/3155257/28124/en/Pharmaceutical-Contract-Research-Services-Market-Report-2025-2035-M-A-Partnerships-and-Biologics-Focus.html]
- 74. Analytical and clinical validation of a high accuracy fully ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1568971/full]
- 75. Resourcing and Outsourcing Trends in Drug Development [https://www.appliedclinicaltrialsonline.com/view/resourcing-outsourcing-trends-drug-development]
- 76. Why Full Service CROs Are Winning in 2025 [https://cromospharma.com/full-service-cros-in-2025/]
- 77. Outsourcing clinical trials: the pros and cons in 2026 [https://clinicaltrialrisk.org/clinical-trial-design/outsourcing-clinical-trials-the-pros-and-cons/]
- 78. A longitudinal cohort study uncovers plasma protein ... [https://www.nature.com/articles/s41467-025-62032-1]
- 79. The Biomarker Evaluation Process - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK220290/]
- 80. Analytical Methodology: Validation, Verification, or ... [https://vicihealthsciences.com/analytical-methodology-validation-verification-qualification/]
- 81. Qualification Vs Validation: Understand The Key Differences [https://gmpinsiders.com/qualification-vs-validation-key-differences/]
- 82. Eligibility criteria - NCATS Toolkit - NIH [https://toolkit.ncats.nih.gov/glossary/eligibility-criteria/]
- 83. What is clinical trial eligibility criteria? [https://www.abbvieclinicaltrials.com/resources/what-are-eligibility-criteria-clinical-trials/]
- 84. Biomarker Qualification Program [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/biomarker-qualification-program]
- 85. Qualification of novel methodologies for medicine development [https://www.ema.europa.eu/en/qualification-novel-methodologies-medicine-development]
- 86. Biomarker Qualification: Evidentiary Framework [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/biomarker-qualification-evidentiary-framework]
- 87. Biomarker Guidances and Reference Materials [https://www.fda.gov/drugs/biomarker-qualification-program/biomarker-guidances-and-reference-materials]
- 88. Comparison of the FDA and EMA guidance on drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12280173/]
- 89. Bioinformatics and experimental validation identify ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1566929/full]
- 90. Experimental verification and validation of immune ... [https://pubmed.ncbi.nlm.nih.gov/36105086/]
- 91. Validity, Accuracy and Reliability: A Comprehensive Guide [https://scienceready.com.au/pages/validity-accuracy-and-reliability?srsltid=AfmBOooigvULk-wYqyRPbStCtlzN4yZcusb9pVmKx2G3bxyNhmjI0MhU]
- 92. Accuracy, precision, specificity & sensitivity [https://labtestsonline.org.uk/articles/accuracy-precision-specificity-sensitivity]
- 93. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 94. Accuracy, Precision, and Reliability of Chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3026088/]
- 95. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 96. An overview of statistical methods for biomarkers relevant ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1351584/full]
- 97. Biomarker Validation: Common Data Analysis Concerns [https://pmc.ncbi.nlm.nih.gov/articles/PMC4122484/]
- 98. Validation Processes of Protein Biomarkers in Serum—A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3478866/]
- 99. Biomarkers and Detection Platforms for Human Health and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8895156/]
- 100. A Comprehensive Oncological Biomarker Framework Guiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466961/]
- 101. Enzymes & Metabolic Biomarker [https://www.centogene.com/diagnostics/enzymes-metabolic-biomarker/]
- 102. Development and clinical validation of blood-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12045422/]
- 103. Identification and experimental validation of biomarkers ... [https://www.nature.com/articles/s41598-025-17606-w]