Optimizing Biomedical Experiments: A Practical Guide to the Fisher Information Matrix for Efficient Drug Development
This article provides a comprehensive guide to the Fisher Information Matrix (FIM) and its pivotal role in optimal experimental design (OED) for biomedical and pharmaceutical research.
Optimizing Biomedical Experiments: A Practical Guide to the Fisher Information Matrix for Efficient Drug Development
Abstract
This article provides a comprehensive guide to the Fisher Information Matrix (FIM) and its pivotal role in optimal experimental design (OED) for biomedical and pharmaceutical research. We first establish the foundational link between the FIM and the precision of parameter estimation via the Cramér-Rao bound, explaining its critical function in model-based design[citation:2][citation:4]. We then explore methodological advancements, including optimization-free, ranking-based approaches for online design and the implementation of population FIMs for nonlinear mixed-effects models prevalent in pharmacokinetics/pharmacodynamics (PK/PD)[citation:1][citation:3]. A dedicated troubleshooting section analyzes the impact of key approximations (FO vs. FOCE) and matrix implementations (Full vs. Block-Diagonal FIM) on design robustness, especially under parameter uncertainty[citation:2]. Finally, we compare validation strategies, from asymptotic FIM evaluations to robust simulation-based methods, offering a clear framework for researchers and drug development professionals to design more informative, cost-effective, and reliable studies.
The Core of Precision: Demystifying the Fisher Information Matrix and the Cramér-Rao Bound
Technical Support Center: FIM Troubleshooting & FAQs
This technical support center is designed for researchers and scientists applying Fisher Information Matrix (FIM) concepts within optimal experimental design (OED), particularly in drug development. The FIM quantifies the amount of information a sample provides about unknown parameters of a model, guiding the design of efficient and informative experiments [1] [2]. Below are common technical issues, troubleshooting guides, and detailed protocols to support your work.
Frequently Asked Questions (FAQs)
Q1: What is the Fisher Information Matrix (FIM), and why is it critical for my experimental design? The FIM is a mathematical measure of the information an observable random variable carries about unknown parameters of its underlying probability distribution [2]. In optimal design, you aim to choose controllable variables (e.g., sample times, dose amounts) to maximize the FIM. This is equivalent to minimizing the lower bound on the variance of your parameter estimates, as defined by the Cramér-Rao Bound (CRB) [3]. A larger FIM indicates your experiment will yield more precise parameter estimates, leading to more robust conclusions from costly clinical or preclinical trials [4].
Q2: My model parameters are highly correlated, leading to a near-singular FIM. What should I do? A near-singular FIM indicates poor parameter identifiability—your data cannot reliably distinguish between different parameter values. This is reflected in large off-diagonal elements in the FIM or its inverse [3].
- Troubleshooting Steps:
- Simplify the Model: Re-evaluate if all parameters are necessary. Fix well-known parameters to literature values if possible.
- Re-design the Experiment: Use FIM-based optimal design before running the experiment. Optimize sampling times or dose levels to reduce correlation. The D-optimality criterion is specifically designed to minimize the overall variance of parameter estimates by maximizing the determinant of the FIM.
- Include Prior Information: If using a Bayesian framework, consider using the prior distribution to regularize the problem. The FIM forms the basis of non-informative priors in Jeffreys' rule [2].
Q3: How do I calculate the FIM for a nonlinear mixed-effects (NLME) model commonly used in pharmacometrics? For NLME models, the marginal likelihood requires integrating over random effects, making exact FIM calculation difficult.
- Standard Protocol: The First Order (FO) approximation is widely used. This method linearizes the model around the expected values of the random effects (typically zero), allowing for an approximate, closed-form calculation of the expected FIM for the population-level parameters [3].
- Important Note: The FO approximation is an estimation. Always validate your final optimal design using stochastic simulation and re-estimation (SSE) to confirm that parameter precision targets are met in practice [3].
Q4: In dose-response studies, how can FIM-based design improve Phase II/III dose selection? Traditional pairwise dose comparisons are limited and contribute to high late-stage attrition [4]. FIM-based OED shifts the paradigm to an estimation problem.
- Application: You design a study to precisely estimate the parameters of a dose-exposure-response (DER) model (e.g., an Emax model). By maximizing the FIM for parameters like Emax (maximum effect) and ED50 (potency), you optimally select dose levels and patient allocation to learn the full dose-response curve. This provides a scientific rationale for selecting the optimal dose for confirmatory trials, rather than just a statistically significant one [4].
Troubleshooting Guides
Issue: Poor Precision in Key Parameter Estimates
- Symptom: After analysis, the confidence intervals for critical parameters (e.g., drug clearance, IC50) are unacceptably wide.
- Diagnosis: The experimental design provided insufficient information for those parameters.
- Solution:
- Pre-Design FIM Evaluation: Before conducting the experiment, compute the expected FIM for your proposed design (sampling schedule, doses, sample sizes) [3].
- Apply an Optimality Criterion: Use a criterion like A-optimality (minimizing the trace of FIM inverse) to improve the average precision of your specific parameters of interest.
- Iterate: Use software tools to optimize your design variables (e.g., times, doses) to maximize your chosen criterion. The table below compares common criteria.
Table 1: Common Optimality Criteria for Experimental Design
| Criterion | Objective | Best Used For | Mathematical Form |
|---|---|---|---|
| D-Optimality | Maximizes overall precision; minimizes joint confidence ellipsoid volume. | General purpose design; model discrimination. | Maximize det(FIM) |
| A-Optimality | Maximizes average precision of individual parameter estimates. | Focusing on a specific set of parameters. | Minimize trace(FIM⁻¹) |
| C-Optimality | Minimizes variance of a linear combination of parameters (e.g., predicted response). | Precise prediction at a specific point (e.g., target dose). | Minimize cᵀFIM⁻¹c |
Issue: Failed Model Convergence or Estimability During Analysis
- Symptom: Software fails to converge or reports "estimability" errors when fitting the model to the collected data.
- Diagnosis: The collected data is information-poor for the chosen model, often due to a suboptimal design. This is a direct consequence of a low FIM.
- Solution:
- Simulate and Verify: Prior to the physical experiment, simulate virtual datasets from your proposed optimal design and your model. Attempt to re-estimate parameters from these datasets.
- Assess Success Rate: If the estimation fails or is biased in >20% of simulations, the design is inadequate despite theoretical FIM optimality [3].
- Re-optimize with Constraints: Add practical constraints (e.g., minimum time between samples, feasible dose levels) and re-optimize the design. A multi-objective framework can balance information with cost and practicality [5].
Detailed Experimental Protocols
Protocol 1: FIM-Based Optimal Design for a Dose-Response Study
This protocol outlines steps to design a dose-finding study using an Emax model.
1. Define the Model and Parameters:
- Model: ( E = E0 + \frac{E{max} \cdot D}{ED_{50} + D} )
- Parameters to Estimate: ( E0 ) (baseline effect), ( E{max} ) (maximum drug effect), ( ED{50} ) (dose producing 50% of ( E{max} )) [4].
- Parameter Uncertainty: Specify initial/prior estimates and their uncertainty (e.g., coefficient of variation).
2. Specify Design Variables and Constraints:
- Variables: Dose levels (D), number of subjects per dose (N), sampling times for response measurement.
- Constraints: Total number of subjects, minimum/maximum safe dose, clinical sampling limitations.
3. Compute and Optimize the Expected FIM:
- Using optimal design software (e.g., Pumas, PopED), calculate the expected FIM for a candidate design [3].
- Select an optimality criterion (see Table 1). For dose-response, D-optimality is often used to precisely estimate all parameters of the curve.
- Run an optimization algorithm to adjust design variables to maximize the criterion.
4. Validate Design via Simulation:
- Simulate 500-1000 virtual trials using the optimal design.
- Fit the Emax model to each simulated dataset.
- Calculate the relative root mean square error (RRMSE) for each parameter: ( \text{RRMSE} = \sqrt{\text{MSE}} / \text{True Value} ). A successful design should have RRMSE < 0.3 for key parameters.
Table 2: Example Dose-Response Parameters and Target Precision
| Parameter | Symbol | Initial Estimate | Target RRMSE | Biological Role |
|---|---|---|---|---|
| Baseline Effect | ( E_0 ) | 10 units | < 0.15 | Disease severity without treatment. |
| Maximum Effect | ( E_{max} ) | 50 units | < 0.25 | Maximal achievable drug benefit. |
| Potency | ( ED_{50} ) | 5 mg | < 0.30 | Indicator of drug strength; key for dose selection. |
5. Implement and Adapt:
- Run the study according to the optimized design.
- For adaptive trials, interim data can be used to update parameter estimates and re-optimize the design for remaining subjects [4].
Protocol 2: Diagnosing & Solving Parameter Non-Identifiability
Symptoms: Extremely large standard errors, failure of estimation algorithm, strong pairwise parameter correlations (>0.95) in the correlation matrix (derived from FIM⁻¹).
Diagnostic Steps:
- Compute the FIM and its Eigenvalues: A singular FIM will have one or more eigenvalues near zero. The corresponding eigenvectors indicate which linear combinations of parameters are not informed by the data.
- Profile Likelihood Analysis: For each parameter, fix it at a range of values and optimize over all others. A flat profile likelihood indicates the data does not contain information about that parameter.
Remedial Actions:
- Design Enhancement: Add informative data points (e.g., a new sampling time, an additional dose level) targeted at the weak directions identified by the FIM eigenanalysis.
- Parameter Reduction: If two parameters are perfectly correlated (e.g., volume and clearance in a simple PK model), consider if they can be combined into a single composite parameter (e.g., half-life).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for FIM-Based Optimal Experimental Design
| Tool/Reagent Category | Specific Example/Function | Role in FIM/OED Research |
|---|---|---|
| Optimal Design Software | Pumas (Julia), PopED (R), PFIM (standalone) | Platforms to compute expected FIM for nonlinear models, optimize designs, and perform validation simulations [3]. |
| Pharmacometric Modeling Software | NONMEM, Monolix, Phoenix NLME | Industry-standard tools for building NLME models. The final model structure is the foundation for FIM calculation. |
| Statistical Computing Environment | R, Python (SciPy), Julia | Essential for custom scripting, advanced statistical analysis, and implementing bespoke optimality criteria or visualizations. |
| Clinical Trial Simulation Framework | Clinical trial simulation (CTS) suites [4] | Used to validate optimal designs under realistic, stochastic conditions beyond the FIM approximation. |
| Reference Models & Parameters | Published PK/PD models (e.g., Emax, indirect response) | Provide initial parameter estimates and uncertainty required to compute the expected FIM before any new data is collected [4]. |
Visual Guides: Workflows and Relationships
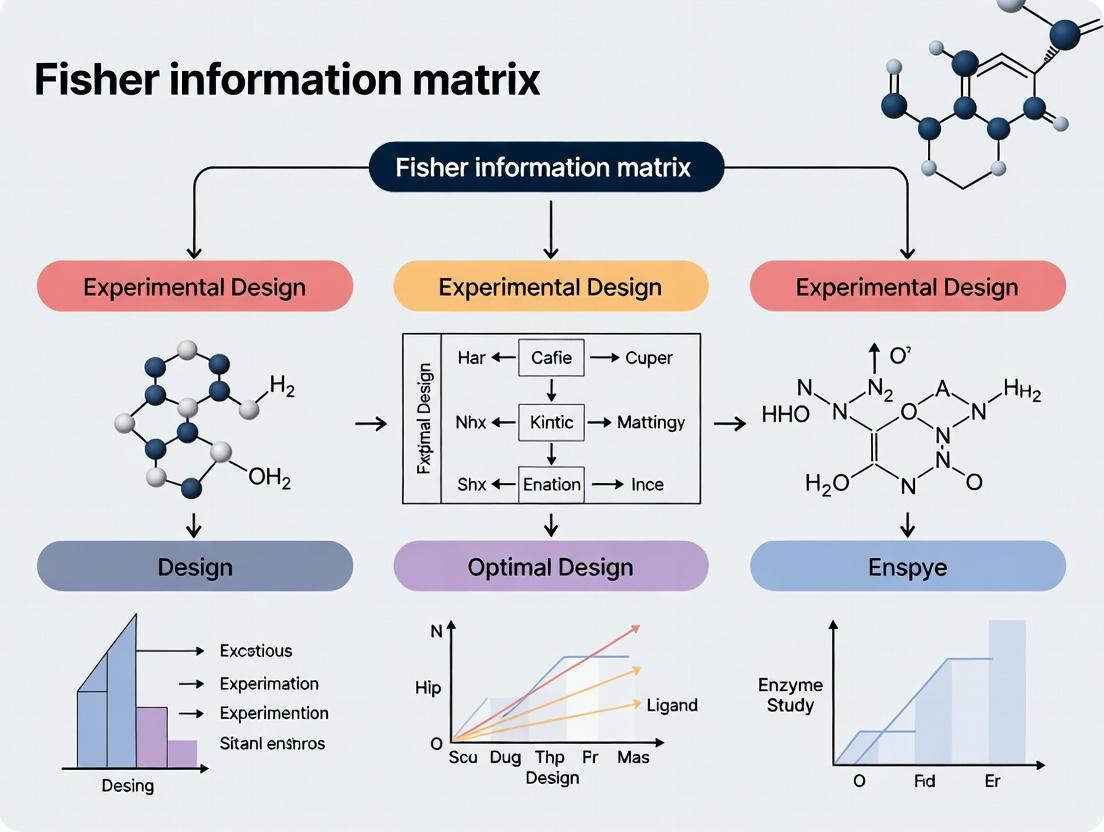
Diagram 1: FIM-Based Optimal Design Cycle (85 characters)
Diagram 2: Integrating PK/PD Models with FIM (74 characters)
In the context of optimal experimental design, a core objective is to configure experiments that yield the most precise estimates of model parameters, such as kinetic constants or drug potency. The Cramer-Rao Bound (CRB) provides the theoretical foundation for this pursuit. It states a fundamental limit: for any unbiased estimator of a parameter vector (\boldsymbol{\theta}), its covariance matrix cannot be smaller than the inverse of the Fisher Information Matrix (FIM) [6] [7]. Formally:
[ \operatorname{Cov}(\hat{\boldsymbol{\theta}}) \succeq I(\boldsymbol{\theta})^{-1} ]
where (I(\boldsymbol{\theta})) is the FIM and (\succeq) denotes that the difference is a positive semi-definite matrix [6]. The FIM quantifies the amount of information an observable random variable carries about the unknown parameters [2]. Therefore, in experiment design, we aim to maximize the FIM (according to a chosen optimality criterion like D-optimality) to push the achievable variance of our estimators toward this theoretical lower bound, ensuring maximal precision [8].
Technical Support Center: Troubleshooting FIM & CRB Applications
FAQ 1: What is the practical interpretation of the Cramér-Rao Bound for my experiment?
The CRB is not just a theoretical limit; it is a direct benchmark for your experimental design's potential efficiency. If you calculate the FIM for your proposed experimental protocol (e.g., sampling times, dosages), its inverse provides a lower bound on the covariance matrix for your parameter estimates. By comparing the actual performance of your estimator against this bound, you can assess how much room for improvement exists. An estimator that attains the bound is called efficient [6] [9]. In pharmacometrics, optimizing designs to maximize the FIM (minimize the bound) is a standard method to reduce required sample sizes and costs [8].
FAQ 2: My optimal design is producing highly clustered sampling points. Is this a problem, and how can I address it?
Issue: Clustering of sampling times or conditions is a common outcome of D-optimal design, where samples are placed at theoretically information-rich points [8]. Troubleshooting: While clustering is optimal for a perfectly specified model, it reduces robustness. If the model structure or prior parameter values are misspecified, clustered designs can perform poorly [8]. Solutions:
- Use a more accurate FIM approximation: Research shows that using the First-Order Conditional Estimation (FOCE) approximation instead of the simpler First-Order (FO) method, along with a full FIM calculation (not block-diagonal), tends to generate designs with more support points and less clustering, enhancing robustness to parameter misspecification [8].
- Implement a robust design criterion: Consider criteria like ED-optimality that account for parameter uncertainty explicitly.
- Apply practical constraints: Enforce minimum time intervals between samples in the optimization algorithm to ensure feasibility and robustness.
FAQ 3: Why do my parameter estimates have higher variance than the CRB predicted? What are the common causes?
The CRB assumes the estimator is unbiased and that the model is correct. Discrepancies arise from:
- Model Misspecification: The CRB is derived for the true underlying model. An incorrect model structure invalidates the bound [8].
- Parameter Misspecification in Design: Using incorrect prior parameter values to compute the FIM during the design phase leads to a suboptimal design that collects less information than predicted [8].
- Violation of Regularity Conditions: The CRB derivation requires conditions like the ability to interchange integration and differentiation [6] [10]. Distributions with parameter-dependent supports (e.g., Uniform(0, θ)) violate these [2].
- Finite Sample Effects: Maximum Likelihood Estimators (MLE) are asymptotically efficient, but for small samples, they may not achieve the bound [9] [7].
- Use of Approximated FIM: In complex nonlinear mixed-effects models (common in drug development), the exact FIM is intractable. Using FO or FOCE approximations introduces error into the bound itself [8].
FAQ 4: The optimization for my model-based design of experiments (MBDoE) is computationally expensive or gets stuck in local optima. Are there alternatives?
Issue: Traditional MBDoE solves a (often non-convex) optimization problem to maximize a function of the FIM, which is computationally intensive and sensitive to initial guesses [11]. Solution: An Optimization-Free FIM-Driven (FIMD) Approach. This emerging methodology [11]:
- Generates a large candidate set of possible experimental conditions.
- For each candidate experiment, computes the FIM based on current parameter estimates.
- Ranks the experiments by an information-theoretic criterion (e.g., D-optimality value).
- Selects the top-ranked experiment for the next run. This iterative, ranking-based approach avoids expensive nonlinear optimization, significantly reduces computation time, and is less prone to local optima, making it suitable for online/autonomous experimental platforms [11].
FAQ 5: When should I use the full FIM versus the block-diagonal FIM in pharmacometric design?
This choice significantly impacts your optimal design [8].
Block-Diagonal FIM: Assumes that the fixed effects parameters ((\beta)) and the variance-covariance parameters ((\lambda)) are independent. It simplifies and speeds up computation [8]. Full FIM: Accounts for the covariance between fixed effects and variance parameters. It is more accurate but computationally heavier [8].
Recommendation: The literature indicates that for design optimization, using the full FIM (especially with the FOCE approximation) generally yields designs that are more robust to parameter misspecification [8]. Use the block-diagonal approximation primarily for initial scoping or when computational resources are severely constrained, acknowledging the potential for increased bias in the resulting designs [8].
Table 1: Comparison of FIM Approximation and Implementation Methods in Pharmacometrics [8]
| Method | Description | Computational Cost | Design Characteristic | Robustness to Misspecification |
|---|---|---|---|---|
| FO Approximation | Linearizes around random effect mean of 0. | Lower | Tends to create designs with clustered support points. | Lower; FO block-diagonal designs showed higher bias. |
| FOCE Approximation | Linearizes around conditional estimates of random effects. | Higher | Creates designs with more support points, less clustering. | Higher. |
| Block-Diagonal FIM | Ignores covariances between fixed & variance parameters. | Lower | Can be less informative. | Generally lower than Full FIM. |
| Full FIM | Includes all parameter covariances. | Higher | More informative support points. | Superior, particularly when combined with FOCE. |
Featured Experimental Protocols
Protocol A: D-Optimal Design for a Pharmacokinetic (PK) Model
This protocol is based on a study optimizing sampling schedules for Warfarin PK analysis [8].
1. Objective: Determine optimal sampling times to minimize the uncertainty (maximize the D-optimality criterion) of PK parameter estimates (e.g., clearance CL, volume V).
2. Pre-experimental Setup:
- Define Model: Use a nonlinear mixed-effects model (e.g., one-compartment, first-order absorption and elimination).
- Specify Parameters: Provide initial (prior) estimates for fixed effects (
CL,V,ka), between-subject variability (BSV), and residual error. - Define Design Space: Specify constraints (e.g., sampling window: 0-72 hours, maximum 10 samples per subject).
3. FIM Calculation & Optimization:
- Select FIM Method: Choose an approximation (FO or FOCE) and implementation (Full or Block-diagonal). For robustness, FOCE with Full FIM is recommended [8].
- Compute FIM: For a given sampling schedule (\xi), calculate the FIM (I(\boldsymbol{\theta}, \xi)) using the chosen method. Software:
PopED,PFIM, orPhoenix. - Optimize: Use an algorithm (e.g., stochastic gradient, exchange) to find the schedule (\xi^*) that maximizes (\log(\det(I(\boldsymbol{\theta}, \xi)))) (D-optimality).
4. Validation via Simulation & Estimation (SSE):
- Simulate 500-1000 datasets using the optimal design (\xi^) and the *true parameter values.
- Estimate parameters from each simulated dataset.
- Calculate the empirical covariance matrix and the empirical D-criterion. Compare this to the predicted FIM-based D-criterion to evaluate performance [8].
Protocol B: Optimization-Free FIMD for Kinetic Model Identification
This protocol implements the FIMD approach for a fed-batch yeast fermentation reactor [11].
1. Objective: Sequentially select the most informative experiment to rapidly reduce uncertainty on kinetic model parameters.
2. Iterative Loop:
- Step 1 - Candidate Generation: At iteration (k), using current parameter estimates (\hat{\boldsymbol{\theta}}_k), generate a large set (S) of candidate experimental conditions (e.g., varying substrate feed rate, temperature).
- Step 2 - FIM Ranking: For each candidate (s \in S), compute the FIM (I(\hat{\boldsymbol{\theta}}_k, s)). Calculate its determinant (D-value).
- Step 3 - Experiment Selection: Choose and run the experiment (s^*) with the highest D-value.
- Step 4 - Parameter Update: Incorporate new data from (s^*), re-estimate parameters to obtain (\hat{\boldsymbol{\theta}}_{k+1}).
- Step 5 - Convergence Check: Stop when parameter confidence intervals are sufficiently small or a set number of iterations is reached.
3. Key Advantage: This method avoids the nonlinear optimization of traditional MBDoE by leveraging ranking, leading to faster convergence and lower computational cost for online applications [11].
Table 2: Key Resources for FIM-based Optimal Experimental Design
| Resource Category | Specific Tool / Solution | Function & Application Note |
|---|---|---|
| Software & Platforms | PopED (R), PFIM, Phoenix NLME, MONOLIX |
Industry-standard platforms for computing FIM and optimizing experimental designs for pharmacometric and biological models. |
| Computational Algorithms | First-Order (FO) & First-Order Conditional Estimation (FOCE) linearization [8] | Algorithms to approximate the FIM for nonlinear mixed-effects models where the exact likelihood is intractable. |
| Statistical Criteria | D-optimality, ED-optimality | Scalar functions of the FIM used as objectives for optimization. D-opt maximizes the determinant of FIM; ED-opt maximizes the expected determinant over parameter uncertainty. |
| Theoretical Benchmarks | Cramér-Rao Bound (Scalar & Multivariate) [6], Bayesian Cramér-Rao Bound [9] | Fundamental limits for unbiased and Bayesian estimators, used to benchmark the efficiency of any estimation procedure. |
| Emerging Methodologies | Fisher Information Matrix Driven (FIMD) approach [11] | An optimization-free, ranking-based method for sequential experimental design, ideal for autonomous experimentation. |
Core Conceptual and Workflow Diagrams
Diagram 1: Logical Pathway from Experiment to Estimation Limit
Diagram 2: Workflow for Model-Based Optimal Design (MBDoE)
The Fisher Information Matrix (FIM) serves as the foundational mathematical bridge connecting a pharmacokinetic/pharmacodynamic (PK/PD) model to the efficiency of an experimental design. In drug development, where studies are costly and subject numbers are limited, optimizing the design through the FIM is critical for obtaining precise parameter estimates with minimal resources [12]. The core principle is encapsulated in the Cramér-Rao inequality, which states that the inverse of the FIM provides a lower bound for the variance-covariance matrix of any unbiased parameter estimator [13] [8]. Therefore, by maximizing the FIM, we minimize the expected uncertainty in our parameter estimates.
This optimization is not performed on the matrix directly but via specific scalar functions known as optimality criteria. The most common is D-optimality, which seeks to maximize the determinant of the FIM, thereby minimizing the volume of the confidence ellipsoid around the parameter estimates [13] [12]. Other criteria, such as lnD- and ELD- (Expected lnD) optimality, provide nuanced approaches for local (point parameter estimates) and robust (parameter distributions) design optimization, respectively [13]. This technical support center addresses the practical challenges researchers encounter when implementing these theoretical concepts, from selecting approximations to validating designs in the context of a Model-Based Adaptive Optimal Design (MBAOD) framework [13].
Technical Support & Troubleshooting Guides
This section provides targeted solutions for common computational, methodological, and interpretive challenges in FIM-based optimal design.
Troubleshooting Guide: Common FIM Implementation Issues
| Problem Category | Specific Symptoms | Probable Cause | Corrective Action & Validation |
|---|---|---|---|
| Parameter Misspecification | Design performs poorly when implemented; high bias or imprecision in parameter estimates from study data. | Prior parameter values (θ) used for FIM calculation are inaccurate [13]. | Implement a Model-Based Adaptive Optimal Design (MBAOD). Use a robust criterion like ELD-optimality, which integrates over a prior parameter distribution [13]. Validate with a pilot study. |
| FIM Approximation Error | Significant discrepancy between predicted parameter precision (from FIM inverse) and empirical precision from simulation/estimation [8]. | Use of an inappropriate linearization method (e.g., First-Order (FO) vs. First-Order Conditional Estimation (FOCE)) for the model's nonlinearity [8]. | For highly nonlinear models or large inter-individual variability, switch from FO to FOCE approximation [8]. Compare the empirical D-criterion from simulated datasets against the predicted value. |
| Suboptimal Sampling Clustering | Optimal algorithm yields only 1-2 unique sampling times, creating risk if model assumptions are wrong. | D-optimality for rich designs often clusters samples at information-rich support points [8]. | Use the Full FIM implementation instead of the block-diagonal FIM during optimization, which tends to produce designs with more support points [8]. |
| Unrealistic Power Prediction | FIM-predicted power to detect a covariate effect is overly optimistic compared to simulation. | FIM calculation did not properly account for the full distribution (discrete/continuous) of covariates [14]. | Extend FIM calculation by computing its expectation over the joint covariate distribution. Use simulation of covariate vectors or copula-based methods [14]. |
| Failed Design Optimization | Optimization routine fails to converge or returns an invalid design. | Numerical instability in FIM calculation; ill-conditioned matrix; inappropriate design space constraints. | Simplify model if possible; check conditioning of FIM; use logarithmic parameterization; verify and broaden design variable boundaries. |
Frequently Asked Questions (FAQs)
Q1: What is the practical difference between D- and lnD-optimality? A1: Mathematically, D-optimality maximizes det(FIM), while lnD-optimality maximizes ln(det(FIM)). They yield the same optimal design because the logarithm is a monotonic function. The lnD form is often preferred for numerical stability, as it avoids computing extremely large or small determinants [13].
Q2: When should I use a robust optimality criterion like ELD instead of local D-optimality? A2: Use a local criterion (D-/lnD-optimality) only when you have high confidence in your prior parameter estimates. If parameters are uncertain (specified as a distribution), a robust criterion (ELD-optimality) that maximizes the expected information over that distribution is superior. Evidence shows MBAODs using ELD converge faster to the true optimal design when initial parameters are misspecified [13].
Q3: How do I choose between FO and FOCE approximations for my model? A3: The First-Order (FO) approximation is faster and sufficient for mildly nonlinear models with small inter-individual variability. The First-Order Conditional Estimation (FOCE) approximation is more accurate for highly nonlinear models or models with large variability but is computationally heavier [8]. Start with FO, but if predicted standard errors seem unrealistic, validate with a small set of FOCE-based optimizations.
Q4: What software tools are available for FIM-based optimal design?
A4: Several specialized tools exist: PFIM (for population FIM), PopED, POPT, and PkStaMP [8]. The MBAOD R-package is designed specifically for adaptive optimal design [13]. The recent work on covariate power analysis has been implemented in a development version of the R package PFIM [14].
Q5: How can I validate an optimal design before running the actual study? A5: Always perform a stochastic simulation and estimation (SSE) study. 1) Simulate hundreds of datasets under your optimal design and true model. 2) Estimate parameters from each dataset. 3) Calculate empirical bias, precision, and coverage. Compare the empirical covariance matrix to the inverse of the FIM used for design [8]. This is the gold standard for performance evaluation.
Detailed Experimental Protocols
Protocol for a Model-Based Adaptive Optimal Design (MBAOD) Study
This protocol outlines the iterative "learn-and-confirm" process for dose optimization, as described in [13].
1. Pre-Study Setup:
- Define PK/PD Model: Specify the structural (e.g., one-compartment PK with sigmoidal Emax PD) and statistical (random effects, residual error) models.
- Set Prior Information: Define initial population parameter estimates (β, ω, σ). Acknowledge potential misspecification (e.g., PD parameters may be 50% overestimated).
- Choose Optimality Criterion: Select lnD-optimality (local) or ELD-optimality (robust) based on parameter certainty.
- Define Stopping Rule: Establish a quantitative endpoint. Example: Stop when the 95% CI for the population mean effect prediction is within 60–140% for all doses and sampling times [13].
- Cohort Design: Determine initial cohort size (e.g., 8 subjects in 2 dose groups) and adaptive cohort size (e.g., +2 subjects per iteration).
2. Iterative MBAOD Loop:
Technical Support Center: Troubleshooting Guides & FAQs
This technical support center provides targeted solutions for common challenges encountered when implementing Fisher Information Matrix (FIM)-based optimal experimental design (OED) in Nonlinear Mixed-Effects (NLME) frameworks. The guidance is framed within a broader thesis on advancing OED to improve the precision and efficiency of pharmacological research and drug development.
Troubleshooting Guide
Issue 1: Singular or Ill-Conditioned Fisher Information Matrix (FIM)
- Symptoms: Software errors stating the FIM is "non-invertible" or "singular"; extremely large or unreliable parameter standard errors from estimation routines; failure of OED optimization algorithms to converge [15].
- Diagnosis: This indicates a practical or structural identifiability problem. Parameters may be unidentifiable due to insufficient data, poor experimental design, or redundant parameterization within the complex NLME model structure [16] [15].
- Solutions:
- Parameter Subset Selection (Leave Out Approach): Systematically identify and fix a subset of problematic parameters to their prior estimates. This reduces the dimensionality of the estimation problem, resulting in a well-conditioned, reduced FIM for designing experiments. Research shows this approach leads to superior designs compared to using a pseudoinverse [15].
- Reparameterize or Simplify the Model: Use prior knowledge or initial exploratory analysis (e.g., profile likelihood) to combine or fix parameters that are highly correlated or cannot be independently informed by the available measurements [16].
- Employ a Sequential Design: Use a two-stage approach. An initial "learning" stage with a safe, conservative design (e.g., a bolus injection) provides data to obtain preliminary parameter estimates. These estimates are then used to compute a stable FIM for optimizing the design of a subsequent "optimization" stage [17].
Issue 2: Poor Practical Identifiability and High Parameter Uncertainty
- Symptoms: Wide confidence intervals for population or individual parameter estimates; parameter estimates that vary significantly with different starting values; inability to distinguish between competing biological hypotheses [16].
- Diagnosis: The experimental design provides insufficient information to precisely estimate all parameters, even if they are structurally identifiable. This is common in NLME models with high inter-individual variability and sparse sampling [16].
- Solutions:
- Adopt a Multi-Start Estimation Approach: Run the parameter estimation algorithm from multiple diverse starting points. Convergence to a single optimum indicates identifiability, while convergence to distinct optima indicates unidentifiability and the need for a better design [16].
- Apply Optimal Design Criteria: Redesign the experiment using FIM-based criteria. Use the initial, uncertain parameter estimates to compute the FIM and optimize the design (e.g., sampling times, dose levels) to maximize a scalar criterion like D-optimality (maximizing determinant) or A-optimality (minimizing trace of the inverse) [17] [18].
- Incorporate Prior Information: Formally use Bayesian optimal design or use the expected FIM integrated over a prior distribution of the parameters. This acknowledges uncertainty upfront and designs experiments that are robust across plausible parameter values [17] [3].
Issue 3: Suboptimal Performance of "Optimal" Designs in Practice
- Symptoms: An experiment designed using OED software yields parameter estimates with higher-than-predicted uncertainty; the optimized design seems impractical or violates clinical constraints.
- Diagnosis: The local approximation (e.g., first-order linearization) used to compute the FIM for the complex NLME model may be inaccurate. The design is only optimal for the specific parameter values used during the design phase [3] [19].
- Solutions:
- Validate with Stochastic Simulation and Estimation (SSE): Before running the costly experiment, simulate hundreds of virtual datasets using the proposed design and the NLME model. Re-estimate parameters from each dataset. The empirical distribution of the estimates will reveal the true, not approximated, expected performance of the design [3].
- Enforce Real-World Constraints Explicitly: Frame the OED problem as a constrained optimization. Include hard limits on total dosage, maximum instantaneous infusion rates, clinically feasible sampling times, and patient/animal safety boundaries directly in the optimization algorithm [17].
- Use More Accurate FIM Approximations: Explore software tools that use more sophisticated methods than first-order linearization to approximate the FIM, such as Monte Carlo sampling to compute the mean response and its covariance matrix [19].
Frequently Asked Questions (FAQs)
Q1: What is the fundamental link between the Fisher Information Matrix (FIM) and the quality of my parameter estimates in an NLME model? A1: The FIM quantifies the amount of information your experimental data provides about the unknown model parameters. According to the Cramér-Rao lower bound, the inverse of the FIM provides a lower bound for the covariance matrix of any unbiased parameter estimator [3]. Therefore, a "larger" FIM (as measured by optimality criteria) translates to a theoretical minimum for parameter uncertainty that is smaller, meaning your estimates can be more precise.
Q2: I understand D-optimality minimizes the generalized variance, but what do A-optimal and V-optimal designs target? A2: Different optimality criteria minimize different aspects of uncertainty:
- A-Optimality: Minimizes the average variance of the parameter estimates (trace of the inverse FIM). It is ideal when you want all parameters to be estimated with good, balanced precision [17] [18].
- V-Optimality: Minimizes the average prediction variance over a set of important experimental conditions. It is used when the primary goal is to make the most accurate future predictions from the model, rather than just estimating parameters [15].
- D-Optimality: Minimizes the volume of the joint confidence ellipsoid for the parameters (determinant of the inverse FIM). It is the most common criterion for improving overall parameter identifiability [18].
Q3: How do I choose initial parameter values for OED when studying a new compound with high inter-subject variability? A3: When prior information is very limited, implement a two-stage sequential design. The first stage uses a simple, safe design (like a moderate bolus) to collect preliminary data from the population. These data are used to obtain initial estimates (a "prior distribution") for the parameters. The FIM is then calculated based on this prior to design an optimized second-stage experiment (e.g., a complex infusion schedule) tailored to reduce the remaining uncertainty [17].
Q4: Can modern AI/ML methods be integrated with FIM-based OED in NLME frameworks? A4: Yes, hybrid approaches are emerging. For instance, AI can be used to model complex, non-specific response patterns (e.g., placebo effect) from historical data. The predictions from the AI model (e.g., an Artificial Neural Network) can then be integrated as covariates or into the error structure of an NLME model. The FIM for this combined "AI-NLME" model is then used for OED, leading to trials with enhanced signal detection for the true drug effect [20]. This represents a cutting-edge extension of traditional FIM methodology.
Detailed Experimental Protocols
Protocol 1: Two-Stage Optimal Design for Pharmacokinetic (PK) Parameter Estimation
- Objective: Precisely estimate individual-specific PK parameters (e.g., clearance, volume of distribution) with minimal data points, subject to safety constraints [17].
- Methodology:
- Learning Stage: Administer a standard, safe bolus injection. Take 4-6 strategic blood samples over the compound's anticipated half-life. Fit an NLME PK model to obtain individual empirical Bayes estimates and their population distribution.
- FIM Computation: Using the individual estimates from Step 1 as the prior
θ, compute the expected FIM for a candidate designd(a vector of future sample times and infusion rates). For a linear(ized) model, the FIM entry(i,j)is a quadratic formI_θ(i,j) = u_agg^T * M_θ(i,j) * u_agg, whereu_aggincludes the input design [17]. - Optimization Stage: Solve a constrained optimization problem:
max_d [ log(det(FIM(θ, d))) ](for D-optimality). Constraints include maximum/minimum infusion rate, total dose, and time horizon. The output is an optimized infusion schedule and sampling plan. - Validation: Perform Stochastic Simulation and Estimation (SSE) with the optimized design to confirm performance.
Protocol 2: D-Optimal Design for Signaling Pathway Model Calibration
- Objective: Identify an optimal dynamic input (e.g., cytokine concentration) profile to minimize parameter uncertainty in a systems biology ODE model [18].
- Methodology:
- Sensitivity Analysis: For the nonlinear ODE model
dx/dt = f(x,u,p), compute local sensitivity coefficientsS_ij = ∂y_i/∂p_jfor all measured outputsyand parameterspat numerous time points. - FIM Construction: Assemble the sensitivity matrix
S. The FIM is approximated byF = S^T * S[18]. - Input Optimization: Parameterize the input
u(t)as a piecewise-constant function. Use an optimization algorithm to maximizelog(det(F))by adjusting the sequence of input levels, subject to bounds (e.g., non-negative, below cytotoxic level). This often results in a pseudo-random binary sequence (PRBS)-like input that dynamically perturbs the system [18]. - In-Silico Validation: Compare the parameter covariance matrix from the optimal dynamic input versus a constant input via simulated experiments.
- Sensitivity Analysis: For the nonlinear ODE model
Data Presentation: Optimality Criteria Comparison
The choice of optimality criterion depends on the primary goal of the experimental design. The table below summarizes key properties [17] [15] [18].
| Optimality Criterion | Mathematical Objective | Primary Goal | Key Advantage |
|---|---|---|---|
| D-Optimality | Maximize det( FIM ) |
Minimize the joint confidence ellipsoid volume for all parameters. | General purpose; promotes overall parameter identifiability. |
| A-Optimality | Minimize trace( FIM⁻¹ ) |
Minimize the average variance of parameter estimates. | Good for balanced precision across parameters. |
| V-Optimality | Minimize trace( W * FIM⁻¹ ) |
Minimize the average prediction variance over a region of interest (matrix W). |
Best for ensuring accurate model predictions. |
| E-Optimality | Maximize λ_min( FIM ) |
Maximize the smallest eigenvalue of the FIM. | Improves the worst-case direction of parameter estimation. |
Visualization: Workflows and Relationships
Diagram 1: FIM-Based Optimal Design Conceptual Workflow (78 chars)
Diagram 2: Two-Stage Sequential Optimal Design Protocol (59 chars)
Diagram 3: AI-NLME Hybrid Analysis & Design Workflow (65 chars)
The Scientist's Toolkit
Essential software, packages, and methodological approaches for implementing FIM-based OED in NLME frameworks.
| Tool / Resource | Type | Primary Function in NLME OED | Key Consideration |
|---|---|---|---|
| Monolix | Software Suite | NLME parameter estimation & simulation. Includes the simulx library for optimal design [16]. |
Industry-standard; user-friendly interface for modeling and simulation. |
| Pumas | Software Suite & Language | NLME modeling, simulation, and built-in optimal design capabilities [3]. | Modern, open-source toolkit with a focus on optimal design workflows. |
| PkStaMp Library | Software Library | Construction of D-optimal sampling designs for PK/PD models using advanced FIM approximations [19]. | Useful for improving FIM calculation accuracy via Monte Carlo methods. |
| Stochastic Simulation & Estimation (SSE) | Methodology | Validates the operating characteristics (bias, precision) of a proposed design before running the experiment [3]. | Critical step to confirm that a locally optimal design performs well in practice. |
| Profile Likelihood / Multistart Approach | Diagnostic Methodology | Assesses practical parameter identifiability by exploring the likelihood surface, complementing FIM analysis [16]. | Essential for diagnosing issues that a singular FIM may indicate. |
| Sequential (Two-Stage) Design | Experimental Strategy | Mitigates the "chicken-and-egg" problem of needing parameters to design an experiment [17]. | Highly practical for studies with high variability and limited prior information. |
From Theory to Practice: Implementing FIM-Driven Design in Biomedical Research
Technical Support Center: Troubleshooting and FAQs
This technical support center is designed within the context of advanced research on optimal experimental design and the Fisher information matrix. It provides targeted guidance for researchers, scientists, and drug development professionals encountering practical challenges when implementing Model-Based Design of Experiments (MBDoE) frameworks for system optimization and precise parameter estimation [21].
Model-Based Design of Experiments (MBDoE) is a systematic methodology that uses a mathematical model of a process to strategically design experiments that maximize information gain for a specific goal, such as precise parameter estimation or model discrimination [21]. Unlike traditional factorial designs, MBDoE leverages current model knowledge and its uncertainties to recommend the most informative experimental conditions [22].
The Fisher Information Matrix (FIM) is central to this framework. For a parameter vector θ, the FIM quantifies the amount of information that observable data carries about the parameters. It is defined as the negative expectation of the Hessian matrix of the log-likelihood function. In practice, for nonlinear models, it is approximated using sensitivity equations. The FIM's inverse provides a lower bound (Cramér-Rao bound) for the variance-covariance matrix of the parameter estimates, making its maximization synonymous with minimizing parameter uncertainty [23].
The following diagram illustrates the sequential workflow of an MBDoE process driven by the Fisher Information Matrix.
Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents, materials, and software tools commonly employed in MBDoE studies, particularly in chemical and biochemical engineering contexts [24] [25] [22].
| Item Name | Category | Function & Application in MBDoE |
|---|---|---|
| gPROMS ProcessBuilder | Software | A high-fidelity process modeling platform used to formulate mechanistic models, perform parameter estimation, and execute MBDoE algorithms for optimal design [22]. |
| Pyomo.DoE | Software | An open-source Python package for designing optimal experiments. It calculates the FIM for a given model and optimizes design variables based on statistical criteria (A-, D-, E-optimality) [26]. |
| Vapourtec R-Series Flow Reactor | Hardware | An automated continuous-flow chemistry system. It enables precise control of reaction conditions (time, temp, flow) and automated sampling, crucial for executing sequential MBDoE protocols [22]. |
| Plackett-Burman Design Libraries | Statistical Tool | A type of fractional factorial design used in initial screening phases to efficiently identify the most influential factors from a large set with minimal experimental runs [25]. |
| Sparse Grid Interpolation Toolbox | Computational Tool | Creates computationally efficient surrogate models for complex, high-dimensional systems. This allows for tractable global optimization of experiments when dealing with significant parametric uncertainty [27]. |
| Definitive Screening Design (DSD) | Statistical Tool | An advanced screening design that can identify main effects and quadratic effects with minimal runs, providing a more informative starting point for optimization than traditional screening designs [25]. |
| Palladium Catalysts (e.g., Pd(OAc)₂) | Chemical Reagent | A common catalyst for cross-coupling and C-H activation reactions often studied using MBDoE to optimize yield and understand complex reaction networks [22]. |
Troubleshooting Common MBDoE Implementation Challenges
Q1: My parameter estimates have extremely high uncertainty or the optimization fails to converge. What could be wrong? This is often a problem of poor practical identifiability, frequently caused by a poorly designed experiment that does not excite the system dynamics sufficiently [22].
- Diagnosis Steps:
- Calculate the FIM for your current experimental design and initial parameter guesses.
- Perform an eigendecomposition of the FIM. The presence of very small eigenvalues indicates that the FIM is ill-conditioned, and certain parameter combinations cannot be uniquely identified from the proposed data [26].
- Solution Protocol (Design-by-Grouping):
- Calculate normalized local parameter sensitivities over the experimental time horizon.
- Group parameters whose sensitivity profiles peak in similar time intervals.
- Use MBDoE to design a separate experiment targeting the precise estimation of each parameter group (e.g., design Experiment A for Group 1 parameters, Experiment B for Group 2) [22].
- Sequentially run these targeted experiments to decouple correlated parameters. This approach was successfully used to estimate kinetic parameters for a C-H activation reaction where full simultaneous estimation was infeasible [22].
Q2: How do I determine the appropriate sample size or number of experimental runs needed for a precise model? Traditional rules of thumb can be insufficient. A modern approach decomposes the Fisher information to link sample size directly to the precision of individual predictions [23].
- Diagnosis: Your model predictions have wide confidence intervals, or performance degrades significantly on validation data.
- Solution Protocol (Five-Step Sample Size Planning):
- Specify the overall outcome risk in your target population.
- Define the anticipated distribution of key predictors in the model.
- Specify an assumed "core model" (e.g., a logistic regression equation with assumed coefficients).
- Use the relationship
Variance(Individual Risk Estimate) ∝ (FIM)^(-1) / Nto decompose the variance of an individual's risk estimate into components from the FIM and sample size (N) [23]. - Calculate the required N to achieve a pre-specified level of precision (e.g., confidence interval width) for predictions at critical predictor values. This method is implemented in software like
pmstabilityss[23].
Q3: Should I use "Classical" MBDoE or Bayesian Optimization (BO) for my problem? The choice depends entirely on the primary objective [28].
- Use Classical MBDoE when:
- Your goal is parameter estimation, model discrimination, or understanding factor effects.
- You have a first-principles or semi-mechanistic model you wish to calibrate.
- You need to account for blocking factors or randomization to avoid time-trend biases [28].
- Use Bayesian Optimization when:
- Your sole goal is to find a global optimum (e.g., maximum yield) of a black-box function.
- You are optimizing hyperparameters of a machine learning model.
- Evaluating the system is extremely expensive, and you need a sample-efficient global search [28].
- Solution: Clearly define your objective. For comprehensive model development and validation, classical MBDoE is essential. BO can be a complementary tool for pure optimization tasks once a model is established.
Q4: The computational cost of solving the MBDoE optimization problem is prohibitive for my large-scale model. Are there efficient alternatives? Yes, this is a common challenge with nonlinear, high-dimensional models. An optimization-free, FIM-driven approach has been developed to address this [29].
- Diagnosis: The nested optimization loop (outer loop: design variables, inner loop: parameter estimation/FIM calculation) is too slow for online or high-throughput application.
- Solution Protocol (FIM-Driven Ranking):
- Define a candidate set of feasible experiments based on practical constraints.
- For each candidate experiment, compute or approximate its expected FIM.
- Rank all candidates based on an optimality criterion (e.g., determinant of FIM).
- Select and run the top-ranked experiment. This sampling-and-ranking method avoids the costly nonlinear optimization step while still providing highly informative designs and has been demonstrated in fed-batch bioreactor and flow chemistry case studies [29].
Detailed Experimental Protocols from Key Studies
The following table summarizes quantitative results and methodologies from pivotal MBDoE implementations, providing a benchmark for experimental design.
Table: Summary of MBDoE Case Studies & Outcomes
| Study Focus | Model & System | MBDoE Strategy | Key Quantitative Result | Reference |
|---|---|---|---|---|
| C-H Activation Flow Process | Pd-catalyzed aziridine formation; 4 kinetic parameters. | Sequential MBDoE with parameter grouping. D-optimal design in gPROMS. | 8 designed experiments with 5-11 samples each reduced parameter confidence intervals by >70% compared to initial DFT guesses [22]. | [22] |
| Benchmark Reaction Kinetics | Consecutive reactions A → B → C in batch; 4 Arrhenius params. |
FIM analysis & A-/D-/E-optimal design via Pyomo.DoE. | Identified unidentifiable parameters from initial data; a designed experiment at T=350K, CA0=2.0M increased min FIM eigenvalue by 500% [26]. | [26] |
| Dynamical Uncertainty Reduction | 19-dimensional T-cell receptor signaling model. | Global MBDoE using sparse grid surrogates & greedy input search. | Designed input sequence & 4 measurement pairs reduced the dynamical uncertainty region of target states by 99% in silico [27]. | [27] |
| Genetic Pathway Optimization | Metabolic engineering for product yield. | Definitive Screening Design (DSD) for screening, followed by RSM. | DSD evaluated 7 promoter strength factors with only 13 runs, correctly identifying 3 key factors for subsequent optimization [25]. | [25] |
Protocol: MBDoE for Kinetic Model Identification in Flow [22]
- Objective: Precisely estimate activation energies (Ea) and pre-exponential factors (k_ref) for a catalytic reaction network.
- Pre-experimental Setup:
- Define Priors: Obtain initial parameter estimates and uncertainties from Density Functional Theory (DFT) calculations or literature.
- Define Constraints: Specify operational bounds (e.g., Tmin, Tmax, concentration limits to avoid precipitation).
- Sequential Experimental Procedure:
- Sensitivity Analysis: Simulate the model with prior parameters to calculate the time-dependent sensitivity coefficients for each parameter.
- Parameter Grouping: Plot normalized sensitivity profiles. Group parameters with maxima in the same time region (e.g., all
k_refparameters). - Design Generation: For a selected parameter group, formulate a D-optimal MBDoE problem to maximize the determinant of the FIM for those parameters. Decision variables are typically initial concentrations, temperature, and sample times.
- Experiment Execution: Implement the designed conditions in an automated flow reactor (e.g., Vapourtec R2+). Use sample loops for precise reagent delivery and an in-line UV cell/GC for analysis.
- Parameter Estimation: Fit the model to the new data, updating only the targeted parameter group.
- Iteration: Update the model with new parameter estimates and uncertainties. Return to Step 1 to design an experiment for the next parameter group. Iterate until all parameter confidence intervals are satisfactorily small.
Advanced Topics: Optimization Frameworks and Future Directions
The field is evolving beyond local FIM-based optimization. The diagram below contrasts the classical local MBDoE approach with a modern global framework designed to manage significant parametric uncertainty.
Future Directions: Research is focusing on hybridizing classical and Bayesian approaches, creating robust designs for large uncertainty sets, and developing open-source, scalable software (like the tools described by Wang and Dowling [24]) to make these advanced MBDoE techniques accessible for broader applications in pharmaceuticals, biomolecular engineering, and materials science [21].
This technical support center is dedicated to the implementation and troubleshooting of the Fisher Information Matrix Driven (FIMD) approach for the online design of experiments (DoE). This method provides an optimization-free alternative to traditional Model-Based Design of Experiments (MBDoE), which relies on computationally intensive optimization procedures that can be prone to local optimality and sensitivity to parametric uncertainty [11].
The core innovation of the FIMD method is its ranking-based selection of experiments. Instead of solving a complex optimization problem at each step, a candidate set of possible experiments is generated. Each candidate is evaluated based on its contribution to the Fisher Information Matrix (FIM), a mathematical measure of the amount of information an observable random variable carries about unknown parameters of a model [2]. The experiment that maximizes a chosen criterion of the FIM (such as the D-criterion) is selected and executed. This process iterates rapidly, allowing for fast online adaptation and reduction of parameter uncertainty in applications such as autonomous kinetic model identification platforms [11].
Diagram 1: Workflow of the FIMD Ranking-Based Approach
Troubleshooting Guide & FAQs
Core Concept & Implementation Issues
Q1: What is the fundamental advantage of the ranking-based FIMD approach over standard MBDoE? The primary advantage is the elimination of the nonlinear optimization loop. Standard MBDoE requires solving a constrained optimization problem to find the single best experiment, which is computationally heavy and can get stuck in local optima. The FIMD method replaces this with a ranking procedure over a sampled candidate set. This leads to a dramatic reduction in computational time per design cycle, enabling true online and real-time experimental design, which is critical for autonomous platforms in chemical and pharmaceutical development [11].
Q2: When generating the candidate set of experiments, what are common pitfalls and how can I avoid them? A poorly designed candidate set will limit the effectiveness of the ranking method.
- Pitfall 1: Poor Coverage. Candidates clustered in a small region of the experimental design space (e.g., time, temperature, concentration) will not provide informative choices.
- Solution: Use a space-filling sampling method (e.g., Latin Hypercube Sampling) to ensure broad and uniform coverage of the allowable operational ranges.
- Pitfall 2: Excessive Size. A very large candidate set makes the ranking calculation inefficient.
- Solution: Determine a sufficient sample size through preliminary tests. A number between 100 and 1000 candidates is often effective, balancing thoroughness with computational speed for online use.
- Pitfall 3: Static Candidates. Using the same fixed candidate set for every iteration.
- Solution: Implement adaptive candidate generation. For example, after several iterations, you can bias the sampling towards regions of the design space that have proven to be more informative.
Fisher Information Matrix Calculation & Approximation
Q3: What are FO and FOCE approximations of the FIM, and which should I use? In nonlinear mixed-effects models common in pharmacokinetic/pharmacodynamic (PK/PD) research, the exact FIM cannot be derived analytically. Approximations are necessary [8].
- First Order (FO): Linearizes the model around the typical parameter values (random effects set to zero). It is computationally fast but can be inaccurate if inter-individual variability is high or the model is highly nonlinear [8].
- First Order Conditional Estimation (FOCE): Linearizes around conditional estimates of the random effects. It is more accurate but computationally more intensive than FO [8].
Selection Guidance: Start with the FO approximation for initial testing and rapid prototyping of your FIMD workflow. For final design and analysis, especially with complex biological models, use the FOCE approximation to ensure reliability. Research indicates that FOCE leads to designs with more support points and less clustering of samples, which can be more robust [8].
Q4: What is the difference between the "Full FIM" and "Block-Diagonal FIM," and why does it matter? This relates to the structure of the FIM when estimating both fixed effect parameters (β) and variance parameters (ω², σ²) [8].
- Full FIM: Accounts for potential correlations between the uncertainty in fixed effects and variance parameters.
- Block-Diagonal FIM: Assumes these uncertainties are independent, simplifying the matrix into two separate blocks.
Impact: Using the block-diagonal approximation is simpler and faster. While studies show comparable performance when model parameters are correctly specified, the full FIM implementation can produce designs that are more robust to parameter misspecification at the design stage [8]. If your initial parameter guesses are poor, the full FIM is the safer choice.
Diagram 2: Key Approximations and Structures of the Fisher Information Matrix
Performance & Validation
Q5: How do I quantitatively validate that my FIMD implementation is working correctly? You should compare its performance against a benchmark. The standard methodology involves simulation and estimation:
- Simulate Data: Use a known model with known ("true") parameters to generate synthetic datasets based on the designed experiments.
- Re-estimate Parameters: Fit the model to each simulated dataset to obtain estimates.
- Calculate Metrics:
- Bias: Difference between the mean of estimated parameters and the true value.
- Precision: Relative Standard Error (RSE%) of the estimates.
- Empirical D-criterion: Calculate the determinant of the inverse empirical variance-covariance matrix from the simulations. A higher value indicates a more informative design [8].
Table 1: Expected Comparative Performance of FIMD vs. Standard MBDoE
| Metric | Standard MBDoE | FIMD (Ranking-Based) | Rationale & Notes |
|---|---|---|---|
| Computational Time per Design Cycle | High | Low (up to 10-50x faster) [11] | FIMD avoids nonlinear optimization. |
| Quality of Final Design | High (when converging to global optimum) | Comparable/High | Ranking on FIM criteria directly targets information gain. |
| Robustness to Initial Guess | Low (risk of local optima) | Higher | Sampling-based candidate generation explores space broadly. |
| Suitability for Online/Real-Time Use | Low | High | Low cycle time enables immediate feedback. |
Experimental Protocols for Method Validation
Protocol 1: Benchmarking on a Fed-Batch Bioreactor
This protocol is based on a published case study for kinetic model identification [11].
- Objective: Estimate the parameters of a Monod-type kinetic model for baker’s yeast fermentation.
- System: Simulated fed-batch reactor. The model includes state equations for biomass, substrate, and product.
- FIMD Implementation:
- Design Variables: Feed flow rate and sampling times for concentration measurements.
- Candidate Generation: Sample 500 candidate feed profiles (piece-wise constant) within operational bounds.
- Ranking Criterion: D-optimality (maximize determinant of FIM).
- Update: After each "experiment" (simulated run), parameters are re-estimated via maximum likelihood.
- Validation: Perform 100 simulation-estimation runs. Compare the mean squared error and parameter identifiability (RSE% < 50%) against designs from a traditional MBDoE optimizer.
Protocol 2: Robustness Test with Parameter Misspecification
This tests the method's performance under realistic conditions of poor initial guesses [8].
- Objective: Design an optimal sampling schedule for a pharmacokinetic (PK) model (e.g., a one-compartment IV bolus model).
- Procedure: a. Use perturbed parameters (e.g., 50% error on clearance and volume) as the initial guess for design. b. Run the FIMD algorithm (using both FO and FOCE approximations) to generate an optimal sampling schedule. c. Evaluate this schedule by simulating data using the true parameters. d. Fit the model to this data multiple times and compute the empirical bias and precision.
- Success Criteria: A robust design will yield low bias (<10%) and acceptable precision (RSE% < 30%) for key parameters (e.g., clearance) even when designed with misspecified values.
Table 2: Key Research Reagent Solutions for FIMD Implementation
| Reagent / Tool | Function in FIMD Research | Technical Notes |
|---|---|---|
| Nonlinear Mixed-Effects Modeling Software (e.g., NONMEM, Monolix, nlmixr) | Provides the environment for defining the mechanistic model, calculating FIM approximations (FO/FOCE), and performing parameter estimation. | Essential for pharmacometric and complex kinetic applications [8]. |
| Scientific Computing Environment (e.g., MATLAB, Python with SciPy/NumPy, R) | Used to implement the core FIMD algorithm: candidate generation, FIM calculation, ranking, and iterative control logic. | Python/R offer open-source flexibility; MATLAB has dedicated toolboxes. |
| D-Optimality Criterion | The scalar objective function for ranking experiments. Maximizing det(FIM) minimizes the volume of the confidence ellipsoid of the parameters. | The most common criterion for parameter precision [11] [8]. |
| Latin Hypercube Sampling (LHS) Algorithm | A statistical method for generating a near-random, space-filling distribution of candidate experiments within specified ranges. | Superior to random sampling for ensuring coverage of the design space. |
| Cramér-Rao Lower Bound (CRLB) | The inverse of the FIM. Provides a theoretical lower bound on the variance of any unbiased parameter estimator. Used to predict best-case precision from a design [2]. | A key metric for evaluating the potential information content of a designed experiment before it is run. |
| Model-Based Design of Experiments (MBDoE) Software (e.g., gPROMS, JMP Pro) | Serves as a benchmark. Its traditional optimization-based designs are used for comparative performance analysis against the FIMD method [11]. | Critical for validating that the FIMD method achieves comparable or superior efficiency. |
Within the framework of optimal experimental design (OED) for nonlinear mixed-effects models (NLMEM), the Population Fisher Information Matrix (FIM) serves as the fundamental mathematical object for evaluating and optimizing study designs in fields like pharmacometrics and drug development [30] [31]. It quantifies the expected information that observed data carries about the unknown model parameters (both fixed effects and variances of random effects). The core objective is to design experiments that maximize a scalar function of the Population FIM (e.g., its determinant, known as D-optimality), thereby minimizing the asymptotic uncertainty of parameter estimates [31].
Prior to the adoption of FIM-based methods, design evaluation relied heavily on computationally expensive Clinical Trial Simulation (CTS), which involved simulating and fitting thousands of datasets for each candidate design [31]. The derivation of an approximate expression for the Population FIM for NLMEMs provided a direct, analytical pathway to predict the precision of parameter estimates, revolutionizing the efficiency of designing population pharmacokinetic/pharmacodynamic (PK/PD) studies [31]. This article establishes a technical support center to empower researchers in successfully implementing these critical computational methods.
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between an Individual FIM and a Population FIM?
- A: The Individual FIM is calculated for a single subject's data given a known set of their individual parameters. The Population FIM, crucial for population design, accounts for the hierarchy of data: it measures the information about the population's typical parameters (fixed effects) and the inter-individual variability (variance of random effects) by integrating over all possible individual parameter realizations given the population model [31].
Q2: Why is the Population FIM only an approximation, and what are the common approximations used?
- A: The exact likelihood for NLMEMs is often intractable. Therefore, approximations are used to calculate the FIM. The most common is the First-Order (FO) linearization approximation, which linearizes the model around the random effects [31]. Some software also offer the First-Order Conditional Estimation (FOCE) approximation, which can be more accurate but is computationally heavier. For most PK/PD models, the FO approximation provides a reliable and efficient balance for design purposes [31].
Q3: My software returns a singular or non-positive definite FIM. What does this mean and how can I fix it?
- A: A singular FIM indicates that your design is insufficient to estimate all parameters—some parameters are non-identifiable under that design. Common causes include [30]:
- Over-parameterization: The model has too many parameters for the proposed data (e.g., sampling times). Simplify the model or add sampling points.
- Poor Design: Sampling times may be clustered, failing to inform certain model dynamics (e.g., absorption vs. elimination). Use optimal design algorithms to find more informative time points.
- Redundant Parameters: Two parameters may be perfectly correlated based on the design. Review parameter correlations in the FIM.
- A: A singular FIM indicates that your design is insufficient to estimate all parameters—some parameters are non-identifiable under that design. Common causes include [30]:
Q4: How do I validate that a design optimized using the predicted FIM will perform well in practice?
- A: The gold standard for validation is Clinical Trial Simulation (CTS). After obtaining an optimal design via FIM maximization, use it as a template to simulate a large number (e.g., 500-1000) of virtual patient datasets. Estimate parameters from each simulated dataset and compare the empirical standard errors of the estimates to the standard errors predicted by the FIM. Close agreement confirms the design's robustness [31].
Q5: What software tools are specifically designed for Population FIM calculation and optimal design?
Troubleshooting Guide: Common Errors and Solutions
| Error / Symptom | Likely Cause | Recommended Action |
|---|---|---|
| Failed convergence of optimization algorithm | Design space is too large or constraints are conflicting; algorithm stuck in local optimum. | 1. Simplify the problem: Reduce the number of variable design parameters [11].2. Use multiple starting points for the optimization.3. Switch optimization algorithms (e.g., from Fedorov-Wynn to a stochastic method). |
| Large discrepancy between FIM-predicted SE and CTS-empirical SE | The FO linearization approximation may be inadequate for a highly nonlinear model at the proposed dose/sampling design. | 1. Switch to a more accurate FIM approximation (e.g., FOCE) if available.2. Use the FIM-based design as a starting point, then refine using a limited, focused CTS [31]. |
| Optimal design suggests logistically impossible sampling times | The optimization is purely mathematical and ignores practical constraints. | 1. Incorporate sampling windows (flexible time intervals) into the optimization.2. Add constraints to force a minimum time between samples or to align with clinic visits. |
| Software crashes when evaluating FIM for a complex ODE model | Numerical instability in solving ODEs or calculating derivatives. | 1. Check ODE solver tolerances and ensure the model is numerically stable.2. Use the software's built-in analytical model library if a suitable approximation exists.3. Simplify the PD model structure if possible. |
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential software "reagents" for performing Population FIM calculations and optimal design [31] [32].
| Software Tool | Primary Function | Key Feature / Application | Access / Reference |
|---|---|---|---|
| PFIM | Design evaluation & optimization for NLMEM. | Implements FO and FOCE approximations; continuous and discrete optimization; R package. | R (CRAN) [32] |
| PopED | Optimal experimental design for population & individual studies. | Flexible for complex models (ODEs), robust design, graphical output; R package. | R (CRAN) [32] |
| POPT / WinPOPT | Optimization of population PK/PD trial designs. | User-friendly interface (WinPOPT); handles crossover and multiple response models. | Standalone [31] |
| PopDes | Design evaluation for nonlinear mixed effects models. | ||
| PkStaMp | Design evaluation based on population FIM. | ||
| IQR Tools | Modeling & simulation suite. | Interfaces with PopED for optimal design; integrates systems pharmacology. | R Package [32] |
| Monolix & Simulx | Integrated PK/PD modeling & simulation platform. | Includes design evaluation/optimization features based on the Population FIM. | Commercial (Lixoft) |
Experimental Protocols and Methodologies
Protocol 1: Evaluating a Candidate Design Using the Population FIM Objective: To assess the predicted parameter precision of a proposed population PK study design.
- Define Pharmacometric Model: Specify the structural PK model (e.g., 1-compartment with oral absorption), statistical model (inter-individual variability on parameters), and residual error model. Fix all parameters to literature-based nominal values [31].
- Define Candidate Design: Specify the design variables: number of subjects (
N), number of samples per subject (n), dose amount (D), and a vector of sampling times (t₁, t₂, ... tₙ). - Compute Population FIM: Use software (e.g., PFIM, PopED) to calculate the FIM using the FO approximation for the given design and model [31].
- Derive Statistics: Calculate the asymptotic variance-covariance matrix as the inverse of the FIM. Extract the Relative Standard Error (RSE %) for each parameter:
RSE% = 100 * sqrt(Cᵢᵢ) / θᵢ, whereCᵢᵢis the diagonal element (variance) for the i-th parameterθᵢ. - Evaluate: A design is generally considered informative if the predicted RSE% for key parameters (e.g., clearance) is below a target threshold (e.g., 30%).
Protocol 2: Validating an Optimal Design via Clinical Trial Simulation Objective: To empirically verify the operating characteristics of a design obtained through FIM-based optimization [31].
- Generate Optimal Design: Using Protocol 1, employ an optimization algorithm (e.g., in PopED) to find the sampling times that maximize the determinant of the FIM (D-optimality).
- Simulate Virtual Trials: Using the optimized design and the same nominal parameter values, simulate
M(e.g., 500) replicates of the full clinical trial dataset, incorporating inter-individual and residual variability. - Estimate Parameters: Fit the pre-specified NLMEM to each of the
Msimulated datasets using a standard estimation tool (e.g., NONMEM, Monolix). - Compare Precision: For each parameter, calculate the empirical standard error as the standard deviation of its
Mestimates. Plot these against the FIM-predicted standard errors. Good agreement (points near the line of unity) validates the FIM approximation and the optimal design's performance.
Visualizing Workflows and Relationships
Diagram: Population FIM Calculation & Design Workflow (100 chars)
Diagram: Online FIM-Driven Experiment Design (100 chars)
Data Presentation: Software and Method Comparisons
Table 1: Comparison of Primary Software Tools for Population FIM & Optimal Design [31] [32]
| Software | Primary Language/Platform | Key Approximation(s) for FIM | Notable Features for Design |
|---|---|---|---|
| PFIM | R | FO, FOCE | Continuous & discrete optimization, library of built-in models. |
| PopED | R | FO, FOCE, Laplace | Highly flexible for complex models (ODEs), robust & group designs. |
| POPT/WinPOPT | Standalone (C++ / GUI) | FO | User-friendly interface, handles crossover designs. |
| PopDes | FO | ||
| PkStaMp | FO |
Table 2: Computational Methods for Fisher Information Matrix Estimation [30]
| Method | Description | Advantages | Limitations / Best For |
|---|---|---|---|
| Analytical Derivation | Exact calculation of derivatives of the log-likelihood. | Maximum accuracy, no simulation noise. | Only possible for simple models with tractable likelihoods. |
| Monte Carlo Simulation | Estimate expectation by averaging over simulated datasets. | General-purpose, applicable to complex models. | Computationally expensive; variance requires many simulations. |
| First-Order Linearization | Approximates NLMEM by linearizing around random effects. | Fast, standard for population PK/PD optimal design. | May be inaccurate for highly nonlinear models in certain regions. |
| Variance-Reduced MC | Uses independent perturbations per data point to reduce noise. | More reliable error bounds with fewer simulations. | Increased per-simulation cost [30]. |
Technical Support Center: Troubleshooting & FAQs
This support center provides solutions for common challenges in Pharmacokinetic/Pharmacodynamic (PK/PD) study design and clinical trial optimization, framed within the context of optimal experimental design and Fisher information matrix research.
Core Concept: Fisher Information in PK/PD Design
The Fisher information matrix (I(θ)) quantifies the amount of information an observable random variable carries about an unknown parameter (θ) of its distribution [2]. In PK/PD, it measures the precision of parameter estimates (e.g., clearance, volume, EC₅₀) from concentration-time and effect-time data. Maximizing Fisher information is the mathematical principle behind optimizing sampling schedules and trial designs to reduce parameter uncertainty.
Troubleshooting Guide: Common PK/PD Study Challenges
Problem 1: Inadequate Data Quality for Model Development
- Symptoms: Poor model fit, high parameter uncertainty, failure to identify significant covariates, model instability.
- Root Cause: Errors in source data, incorrect NONMEM data formatting, or incomplete data handling rules [33].
- Solution - Implement a Quality Control (QC) Checklist:
- Pre-Modeling QC: Verify units, date/time consistency, and handling of missing/blinded data in source datasets [33].
- Input QC: Ensure NONMEM data files have correct
CMT(compartment) values, appropriateEVID(event identity) codes, and that numeric fields are correctly formatted [33]. - Prospective Planning: Develop a detailed Data Analysis Plan (DAP) specifying handling of outliers, covariates for testing, and model discrimination criteria before analysis begins [33].
Problem 2: Suboptimal or Sparse Sampling Schedules
- Symptoms: Inability to characterize absorption or elimination phases, high inter-individual variability (IIV) estimates, poor extrapolation.
- Root Cause: Sampling times chosen based on logistical convenience rather than information content.
- Solution - Apply D-Optimal Design Based on Fisher Information:
- Develop a preliminary model (e.g., from preclinical data or literature).
- Calculate the Fisher Information Matrix for this model for a candidate sampling schedule.
- Use software (e.g., PopED, PFIM) to optimize the schedule by maximizing the determinant of the Fisher Information Matrix (
det(I(θ))), which minimizes the overall variance of parameter estimates. - For population designs, optimize over both number of subjects and sampling times per subject to balance information gain with operational burden.
Problem 3: High Unexplained Variability (Residual Error)
- Symptoms: Large
EPS(epsilon) estimates, wide prediction intervals, poor model predictive performance. - Root Cause: Unaccounted for biological complexity (e.g., target-mediated drug disposition, disease progression) or measurement error.
- Solution - Strategic Model Enhancement:
- Diagnose: Use visual predictive checks (VPCs) to see if error is constant, proportional, or time-dependent.
- Integrate Biology: Consider mechanistic PD models (e.g., indirect response, turnover) informed by literature to replace simple
Emaxmodels [34]. - Leverage AI/ML: Use machine learning to analyze high-dimensional data (genomic, proteomic) to identify novel covariates contributing to variability, which can then be incorporated into the structural model [35].
Problem 4: Failed Translation from Preclinical to Clinical Outcomes
- Symptoms: Human efficacious dose poorly predicted from animal models, unexpected safety profile.
- Root Cause: Over-reliance on PK surrogates (e.g., plasma concentration) without understanding target engagement and downstream biological pathway dynamics [34].
- Solution - Implement Early Model-Based Target Pharmacology Assessment (mTPA):
- Build a physiology-based PK/PD (PBPK/PD) or quantitative systems pharmacology (QSP) framework early in discovery [34].
- Incorporate in vitro target binding and cell system data with in vivo PK to simulate target occupancy and effect timelines.
- Use this framework to define the optimal drug property profile (e.g., required
Cmin,AUC) for medicinal chemistry teams [34].
Frequently Asked Questions (FAQs)
Q1: How can I design a more efficient clinical trial for a diverse patient population?
- Answer: Utilize Model-Informed Drug Development (MIDD) and population PK/PD modeling [36].
- Design Phase: Use your PK/PD model and Fisher information to simulate trials. Optimize sample size and sampling across subgroups (different weights, renal function) to ensure precise parameter estimation for all key subpopulations.
- Analysis Phase: Pool data across phases and conduct a population analysis to formally quantify the impact of intrinsic (age, race, genetics) and extrinsic (concomitant meds) factors on PK and PD [36]. This can support dosing recommendations for broad populations and potentially waive dedicated studies in some groups.
Q2: My drug has complex kinetics (e.g., non-linear, target-mediated). How can I improve my model?
- Answer: Move from empirical to more mechanistic modeling and consider AI/ML augmentation.
- Hybrid Modeling: Develop a mechanistic base structure (e.g., incorporating known target biology) and use non-parametric ML methods to capture patterns residual to this structure [35]. This balances biological plausibility with data-driven flexibility.
- AI-Enhanced Workflows: Use ML for automated model selection among complex alternatives, or to guide parameter estimation where traditional methods fail [35].
Q3: How do I justify a model-based study design to regulators?
- Answer: Demonstrate robustness through rigorous qualification and validation.
- Documentation: Maintain a comprehensive audit trail from the Data Analysis Plan (DAP) through all QC steps [33].
- Validation: Perform internal validation (e.g., bootstrap, visual predictive check) and external validation if possible. For AI/ML components, focus on "explainable AI" techniques to ensure transparency [35].
- Prospective Utility: Show how the model and optimized design directly address a specific development question (e.g., dose selection for a pediatric population) [36].
Key Experimental Protocols
Protocol 1: Fisher Information Maximization for Optimal Sampling Design
- Objective: Identify the sampling time points that minimize the uncertainty of key PK/PD parameter estimates.
- Materials: Preliminary parameter estimates, variance model, software capable of optimal design (e.g., PopED).
- Methodology:
- Specify a base structural PK/PD model (e.g., 2-compartment PK with
EmaxPD). - Define the parameter vector (θ) and its prior estimates (e.g., CL, V,
Emax, EC₅₀). - Define the sampling design domain (e.g., possible time windows from 0 to 24h post-dose).
- Calculate the Fisher Information Matrix
I(θ)for a given design. For a population model withNsubjects,I(θ)sums individual information matrices. - Maximize the
det(I(θ))(D-optimality criterion) by adjusting the number and timing of samples within operational constraints. - Evaluate design robustness to prior parameter misspecification.
- Specify a base structural PK/PD model (e.g., 2-compartment PK with
Protocol 2: Quality Control for Population PK/PD Analysis [33]
- Objective: Ensure the accuracy and reproducibility of modeling results submitted for regulatory decision-making.
- Materials: Source data, NONMEM control streams, output files, post-processing scripts (e.g., in R).
- Methodology:
- Transformation Task 1 (Data): QC the source data and the derived NONMEM dataset. Check consistency of dosing records, time variables, and biomarker values.
- Transformation Task 2 (Modeling): QC the control stream for syntax errors, accurate model code, and appropriate estimation methods. Verify output listings for successful minimization and reasonable parameter estimates.
- Transformation Task 3 (Reporting): QC all post-processing scripts. Ensure figures and tables in the report are correctly generated from the final model outputs.
- An independent pharmacometrician should perform QC checks at each stage. Any error requires correction and re-execution of subsequent steps [33].
Visualizations: Workflows and Relationships
Diagram Title: Fisher Information Workflow for PK/PD Study Optimization
Diagram Title: Quality Control Process for Population PK/PD Analysis [33]
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in PK/PD Studies | Relevance to Optimal Design |
|---|---|---|
| Optimal Design Software (e.g., PopED, PFIM) | Computes Fisher Information Matrix and optimizes sampling schedules, dose levels, and population allocation to maximize information [2]. | Directly implements D-optimality and related criteria to minimize parameter uncertainty. |
| Population Modeling Software (e.g., NONMEM, Monolix) | Fits nonlinear mixed-effects models to sparse, pooled data. Used for final analysis and to obtain prior parameter estimates for design optimization. | Output (parameter estimates, variance) forms the prior θ for Fisher information calculation in the next study design. |
| PBPK/PD Platform (e.g., GastroPlus, Simcyp) | Mechanistically simulates ADME and effect by incorporating in vitro data and physiological system details [34]. | Provides a strong, biologically-informed prior structural model, improving the reliability of Fisher information-based optimization. |
| Explainable AI/ML Tools | Identifies complex covariates and patterns in high-dimensional data (genomics, biomarkers) to reduce unexplained variability [35]. | Reduces residual error in the model, thereby increasing the information content (I(θ)) of concentration and effect measurements. |
| Data QC & Audit Scripts (e.g., in R, Python) | Automates verification of dataset formatting, unit consistency, and plotting for visual QC [33]. | Ensures the data used for model building and Fisher information calculation is accurate, protecting the validity of the entire model-informed process. |
Navigating Pitfalls: Approximations, Robustness, and Advanced FIM Considerations
Frequently Asked Questions (FAQ)
Q1: What is the fundamental difference between the FO and FOCE linearization methods in NLME modeling? A1: The core difference lies in the point of linearization. The First-Order (FO) method linearizes the nonlinear model around the population mean, setting all random effects (η) to zero. In contrast, the First-Order Conditional Estimation (FOCE) method linearizes the model around the conditional modes (the empirical Bayes estimates) of the random effects for each individual [37]. This makes FOCE a more accurate but computationally intensive approximation, as it requires estimating individual η values iteratively.
Q2: When should I use FO instead of FOCE, or vice-versa? A2: Use the FO method for initial model building, screening, or with very simple models when computational speed is critical. It is the fastest and most robust for convergence but provides the poorest statistical quality in terms of bias [38]. The FOCE method is the current standard for final model estimation and inference when data are rich or models are moderately complex. It offers significantly improved accuracy over FO, especially for models with high inter-individual variability or nonlinearity [39]. FOCE is generally recommended for covariate testing and model selection [40].
Q3: What are the main computational and diagnostic advantages of using a FOCE-based linearization approach? A3: A FOCE-based linearization provides a powerful diagnostic tool with major speed advantages. Once the base model is linearized using FOCE, testing extensions (like additional random effects or covariate relationships) on the linearized model is orders of magnitude faster than re-estimating the full nonlinear model [41]. This allows for rapid screening of complex stochastic components or large covariate matrices. The method is also less sensitive to the "shrinkage" of empirical Bayes estimates, which can distort diagnostic plots [41] [40].
Q4: How is the Fisher Information Matrix (FIM) related to these linearization methods in optimal experimental design? A4: In optimal design for NLME models, the population FIM is used to predict parameter uncertainty and the power to detect significant effects (like covariates) [14]. Computing the exact FIM is intractable, so it is approximated using linearization—typically FO linearization. The appropriateness of this FO-linearized FIM has been evaluated, showing it provides predicted errors close to those obtained with more advanced methods, making it a valid and efficient tool for designing population studies [42].
Q5: What software tools commonly implement these methods, and what is PsN's role? A5: NONMEM is the industry-standard software that implements FO, FOCE, and related estimation algorithms [41] [40]. PsN (Perl-speaks-NONMEM) is a crucial toolkit that facilitates and automates many advanced modeling workflows, including the execution of linearization diagnostics [41]. For optimal design, the PFIM software (and its R package) uses the FO-linearized FIM for design evaluation and optimization [42] [14].
Troubleshooting Guides
Issue 1: Long Run Times for Complex Model Building
Problem: Testing multiple random effect structures or covariate relationships on a complex NLME model takes days or weeks, hindering development. Solution: Implement a FOCE linearization screening step.
- Develop and finalize your structural base model using the standard FOCE method in NONMEM.
- Use tools (e.g., in PsN) to generate the linearized version of this base model. This extracts individual predictions (IPRED) and partial derivatives [40].
- Perform your extensive search (e.g., adding multiple random effects, testing a large variance-covariance block, or screening dozens of covariates) on the linearized model.
- The linearized estimation will complete in minutes to hours instead of days, as it avoids repeated integration [41].
- Take the top candidate models from the linearized screening and validate them by re-estimating them as full nonlinear models. This hybrid approach dramatically accelerates model development.
Performance Comparison: Linearized vs. Nonlinear Estimation Table 1: Representative runtime reductions using FOCE linearization for model diagnostics.
| Task / Dataset | Nonlinear Model Runtime | Linearized Model Runtime | Speed Increase (Fold) | Source |
|---|---|---|---|---|
| Testing 4 covariate relations (Tesaglitazar) | 152 hours | 5.1 minutes | ~1800x | [40] |
| Testing 15 covariate relations (Docetaxel) | 34 hours | 0.5 minutes | ~4000x | [40] |
| Diagnosing stochastic components (General) | Variable (Long) | Variable (Short) | 4x to >50x | [41] |
Issue 2: Unstable Convergence or Parameter Bias with FO Method
Problem: An FO-run model converges quickly, but parameter estimates (especially for variability) seem biased or unrealistic, or the model fails validation. Diagnosis: This is a common limitation of the FO approximation. It assumes linearity at η=0, which is often poor when inter-individual variability is high or the model is strongly nonlinear, leading to biased estimates [38]. Solution:
- Always refine with FOCE: Consider FO estimates as initial values. Switch to FOCE (with interaction, FOCE-I, if needed) for the final estimation.
- Assess Bias: For critical projects, conduct a simulation-estimation study: simulate data from your FO-estimated model and re-estimate using FO and FOCE. Compare the average estimates to the true simulation parameters to quantify FO bias [39].
- Use Advanced Methods for Complex Models: For highly nonlinear models (e.g., certain PKPD, TMDD, or PBPK models) or with sparse data, consider moving beyond FOCE to expectation-maximization (EM) methods like SAEM, which can be more robust and accurate, though often slower [39].
Issue 3: Inaccurate Power Prediction for a Planned Study Using FIM
Problem: The predicted power or sample size from an optimal design tool (using FO-linearized FIM) does not match the empirical power from subsequent studies. Potential Causes and Checks:
- Model Misspecification in Design: The FIM calculation is based on a prior model. An incorrect or oversimplified prior model will lead to inaccurate predictions. Re-evaluate your prior parameter and variability estimates.
- Limitations of FO Linearization for FIM: While the FO-linearized FIM is generally appropriate [42], its accuracy can degrade for highly nonlinear models in the intended design. For critical designs, validate by:
- Computing the FIM using a more accurate method (like a linearization around conditional estimates) if available.
- Performing a small-scale simulation study: simulate 100-200 datasets from the prior model under the proposed design, estimate the covariate effect in each, and calculate the empirical power. Compare this to the FIM-based prediction.
- Covariate Distribution: Recent advances allow the FIM's expectation to account for the joint distribution of covariates (discrete/continuous, using copulas), improving power prediction accuracy [14]. Ensure your design software uses the most appropriate method for covariate handling.
Experimental Protocols
Protocol 1: Implementing FOCE Linearization for Covariate Screening
This protocol automates the rapid testing of covariate-parameter relationships [40].
1. Base Model Estimation
- Software: NONMEM with PsN.
- Action: Estimate the final structural model with stochastic components using the
FOCE-Imethod. Ensure successful convergence and reasonable diagnostics. - Output: A converged NONMEM output file (
.lstor.ext).
2. Linearized Base Model Creation
- Tool: PsN's
linearizecommand [41]. - Action: Execute the command on your base model control stream. This tool modifies the control stream to output the individual predictions (IPRED) and the partial derivatives of the model with respect to parameters (ε) and random effects (η).
- Output: A new linearized control stream and associated dataset.
3. Covariate Model Testing on Linearized System
- Action: Write a new control stream that reads the outputs from Step 2 (IPRED, derivatives). In this stream, implement the candidate covariate relationships (e.g.,
CL = θ₁ * (WT/70)^θ₂). The estimation in this step only involves the covariate effect parameters (θ₂), as the base model's structural and stochastic parts are "fixed" via the linearization. - Execution: Run this linearized covariate model. The estimation will complete very rapidly.
- Output: Objective Function Value (OFV) for each covariate model.
4. Model Selection and Validation
- Analysis: Calculate the difference in OFV (ΔOFV) between the base and each covariate model. A ΔOFV < -3.84 (χ², 1 df, α=0.05) suggests significance.
- Validation: Re-estimate the top 2-3 most significant covariate models as full nonlinear models (returning to Step 1 with the covariate included) to confirm the finding and obtain final unbiased parameter estimates.
Protocol 2: Evaluating FO vs. FOCE Performance via Simulation-Estimation
This protocol assesses the bias and precision of estimation methods in a controlled setting [39].
1. Simulation Design
- Software: R, MATLAB, or specialized tools linked with NONMEM/PFIM.
- Action: Design a simulation study based on a known model (e.g., a one-compartment PK model).
- Define fixed parameters (e.g., CL, V).
- Define random effects distributions (Ω for IIV, Σ for residual error).
- Define a sampling schedule (rich: 5-10 points; sparse: 2-3 points).
- Set the number of subjects and the number of simulated datasets (e.g., N=50, sim=500).
2. Data Generation
- Action: For each simulated dataset, generate individual parameters by sampling η from N(0, Ω). Simulate observations using the structural model and adding residual noise according to Σ.
3. Model Estimation
- Action: For each simulated dataset, estimate the model parameters using:
- a) FO method
- b) FOCE method
- c) (Optional) An EM method (e.g., SAEM)
- Record parameter estimates and standard errors for each run.
4. Performance Metrics Calculation
- Analysis: For each parameter and estimation method, calculate across all successful runs:
- Relative Bias (%):
100 * (mean(estimate) - true value) / true value - Relative Root Mean Square Error (RRMSE, %):
100 * sqrt(mean((estimate - true value)^2)) / true value - Convergence Rate (%): Successful runs / Total simulations.
- Relative Bias (%):
- Conclusion: Compare metrics. FO is expected to show higher bias for random effects parameters, especially with sparse data. FOCE should provide more accurate and precise estimates.
Visualizations
FOCE Linearization Workflow for Model Development
FO-Linearized FIM in Optimal Experimental Design
The Scientist's Toolkit
Table 2: Essential Software and Resources for FO/FOCE Linearization and Optimal Design Research.
| Item | Category | Primary Function | Key Role in Approximation Research |
|---|---|---|---|
| NONMEM | Estimation Software | Industry-standard for NLME modeling. Implements FO, FOCE, Laplacian, and EM algorithms. | The primary engine for performing both nonlinear estimation and generating outputs needed for linearization [41] [40]. |
| PsN (Perl-speaks-NONMEM) | Toolkit / Wrapper | Automates and facilitates complex NONMEM workflows, model diagnostics, and bootstrapping. | Contains the linearize command to automate the creation of linearized models for fast diagnostics [41]. |
| PFIM | Optimal Design Software | R package for design evaluation and optimization in NLME models. | Uses the FO-linearized Fisher Information Matrix to compute predicted parameter uncertainty and power for a given design, critical for planning efficient studies [42] [14]. |
| Monolix | Estimation Software | Provides SAEM algorithm for NLME model estimation. | Offers an alternative, robust estimation method (SAEM) for complex models; used as a benchmark to evaluate the accuracy of linearization-based FIM calculations [42]. |
| R / Python with Matrix Libraries | Programming Environment | Custom scripting, simulation, and data analysis. | Essential for conducting custom simulation-estimation studies to evaluate the performance (bias, precision) of FO vs. FOCE methods under different conditions [39]. |
| Xpose / Pirana | Diagnostics & Workflow | Model diagnostics, run management, and visualization. | Supports the model development process that incorporates linearization diagnostics, helping to manage and visualize results from multiple model runs [41]. |
In the field of optimal experimental design (OED) for drug development, the Fisher Information Matrix (FIM) is a critical mathematical tool used to predict the precision of parameter estimates from a proposed study [8]. Maximizing the FIM leads to designs that minimize parameter uncertainty, thereby improving the informativeness and cost-effectiveness of clinical trials [8]. A central technical decision researchers face is the choice of FIM implementation: the Full FIM or the Block-Diagonal FIM. This technical support center is framed within a broader thesis on OED research and provides targeted troubleshooting guidance for scientists navigating these complex matrix implementation choices [43] [8].
Troubleshooting Guides & FAQs
FAQ 1: Why does my optimal design produce heavily clustered sampling times, and how can I get a more practical schedule?
Problem: Your D-optimal design algorithm outputs a schedule where many samples are clustered at just a few time points, making the design logistically difficult or biologically implausible to execute.
Root Cause: This clustering effect is strongly influenced by the interaction between the FIM implementation and the model linearization method (FO or FOCE) used during optimization [8]. Designs optimized using the FO approximation combined with a Block-Diagonal FIM are particularly prone to generating fewer unique "support points" (sampling times) [43] [8].
Solution: To achieve a design with more distributed sampling points:
- Switch your FIM implementation: Use the Full FIM during optimization. Research shows that the Full FIM implementation, especially when paired with the FOCE approximation, consistently yields designs with more support points and less clustering [8].
- Refine your model approximation: If computationally feasible, use the FOCE (First Order Conditional Estimation) linearization instead of FO. The FOCE method provides a more accurate approximation for models with notable nonlinearity or high between-subject variability, which directly impacts the FIM calculation and leads to more spread-out optimal times [8].
- Impose practical constraints: Use your OED software to add explicit constraints on the minimum allowed time between samples or designate a set of allowed sampling windows.
Supporting Evidence: Table 1: Impact of FIM and Approximation Choice on Design Clustering (Support Points)
| FIM Implementation | Model Approximation | Typical Number of Support Points | Clustering Tendency |
|---|---|---|---|
| Block-Diagonal | FO (First Order) | Lower | Higher [8] |
| Full | FO | Intermediate | Moderate [8] |
| Block-Diagonal | FOCE | Intermediate | Moderate [8] |
| Full | FOCE | Higher | Lower [8] |
FAQ 2: My design performed well in theory but poorly in practice. Did my FIM choice lead to biased parameter estimates?
Problem: A design optimized and evaluated using the FIM showed excellent predicted precision. However, when the study data were analyzed, parameter estimates showed significant bias or higher-than-expected uncertainty.
Root Cause: The discrepancy may stem from model parameter misspecification during the design stage. If the initial parameter values used to compute the optimal design are incorrect, the resulting design can be suboptimal. The Block-Diagonal FIM under the FO approximation has been shown to produce designs that are less robust to such initial parameter misspecification, leading to higher bias in final estimates [43] [8].
Solution:
- Assess robustness during design: Conduct a robustness analysis or a parameter uncertainty analysis. Optimize your design not for a single "best guess" of parameters, but over a distribution of possible values. The Full FIM implementation has demonstrated superior performance under conditions of parameter misspecification [8].
- Validate with simulation: Before finalizing the design, perform a Monte Carlo Simulation and Estimation (MCSE) study. Simulate hundreds or thousands of virtual trials using your proposed design and a range of plausible parameter values, then re-estimate the parameters from the simulated data. This provides an empirical measure of expected bias and precision, independent of FIM approximation choices [8].
- Choose a robust FIM: For problems where initial parameter uncertainty is high, prioritize using the Full FIM implementation for optimization, as it has been shown to generate more robust designs under these conditions [8].
Supporting Evidence: Table 2: Performance Under Parameter Misspecification
| Scenario | Recommended FIM Implementation | Key Advantage |
|---|---|---|
| Parameters well-known | Block-Diagonal or Full | Comparable performance; Block-Diagonal may be faster [8] [44]. |
| High parameter uncertainty / Risk of misspecification | Full FIM | Produces designs that maintain lower bias and better precision when initial guesses are wrong [43] [8]. |
FAQ 3: How do I choose between Full and Block-Diagonal FIM for my specific PK/PD model?
Problem: You are unsure which FIM implementation is most appropriate and reliable for your pharmacokinetic/pharmacodynamic (PK/PD) model, balancing accuracy, computational speed, and software compatibility.
Decision Logic: The choice involves a trade-off between theoretical completeness, computational efficiency, and empirical performance.
Understand the Difference:
- Full FIM: Accounts for all correlations between fixed effect parameters (
β) and variance parameters (ω²,σ²). It is the more theoretically complete representation [8]. - Block-Diagonal FIM: Makes the assumption that the variance of the model is independent of changes in the typical values. This simplifies the matrix by setting the covariance blocks between fixed and variance parameters to zero, often speeding up computation [8].
- Full FIM: Accounts for all correlations between fixed effect parameters (
Follow Empirical Evidence: Comparative studies using real-world PK and PKPD models (e.g., warfarin PK, pegylated interferon PKPD) have found that the simpler Block-Diagonal FIM often provides predicted standard errors (SEs) that are closer to empirical SEs obtained from full simulation studies [44].
Consider Computational Burden: For very complex models with many parameters, the Block-Diagonal FIM can offer significant computational advantages during the iterative optimization process.
Recommendation: For most standard population PK/PD models, starting with the Block-Diagonal FIM is a pragmatic and well-validated choice [44]. Reserve the Full FIM for cases where model structure suggests strong interdependence between fixed and random effects, or when conducting robustness analyses for high-stakes designs under significant parameter uncertainty [8].
FAQ 4: The standard errors predicted by my design software don't match simulation results. Is this a bug?
Problem: The asymptotic standard errors predicted by your optimal design software (based on the inverse of the FIM) are consistently different from the empirical standard errors calculated from a simulation-estimation study.
Root Cause: This is likely not a software bug, but a fundamental characteristic of FIM approximations. The FIM provides a lower bound for the parameter variance-covariance matrix, but different approximations (FO vs. FOCE) and implementations (Full vs. Block-Diagonal) lead to different predictions [8]. The Block-Diagonal approximation has been noted in cross-software comparisons to yield predictions that often align better with simulation results [44].
Troubleshooting Steps:
- Consistency Check: Ensure the same model approximation (FO/FOCE) is used for both the FIM-based prediction and the estimation method in your simulation study. Inconsistency here is a common source of discrepancy.
- Benchmark with Literature: For common model types (e.g., one-compartment PK), consult published comparisons like those involving PFIM, PopED, or POPT [44]. They show that while all major software tools give similar relative results, absolute SE predictions will vary based on the embedded FIM method.
- Use Simulation as the Gold Standard: For final design validation, rely on the Monte Carlo Simulation/Estimation (MCSE) procedure. Calculate an empirical D-criterion confidence interval from the simulated data to objectively compare competing designs, as this method is independent of FIM approximation choices [8].
Diagram 1: Logic for Choosing a FIM Implementation (76 chars)
Detailed Experimental Protocols from Key Studies
The core insights in this guide are derived from rigorous methodological research. Below is a detailed protocol based on the seminal study that compared FIM implementations [8].
Protocol: Evaluating Full vs. Block-Diagonal FIM Performance in Optimal Design
1. Objective: To investigate the impact of Full and Block-Diagonal FIM implementations, combined with FO and FOCE model approximations, on the performance and robustness of D-optimal sampling designs.
2. Software & Tools: The study utilized optimal design software capable of computing both FIM types (e.g., PopED or similar). Analysis required nonlinear mixed-effects modeling software (e.g., NONMEM) for simulation-estimation.
3. Experimental Models:
- Example 1: A Warfarin PK model (one-compartment, first-order absorption, linear elimination).
- Example 2: A more complex Pegylated Interferon PKPD model for hepatitis C viral dynamics [44].
4. Procedure:
- Step 1 - Design Optimization: For each model, generate four D-optimal sampling designs by crossing two factors:
- FIM Implementation:
Fullvs.Block-Diagonal. - Model Approximation:
FOvs.FOCE.
- FIM Implementation:
- Step 2 - Design Analysis: Compare the structural properties of each optimal design, specifically the number of unique support points (sampling times).
- Step 3 - Performance Evaluation (Simulation):
- Simulate several hundred virtual trials using the true model parameters and each optimized design.
- For each simulated trial, estimate the model parameters.
- From the set of estimates, calculate the empirical bias and the empirical variance-covariance matrix.
- Step 4 - Robustness Testing: Repeat Step 3, but simulate data using a different set of parameter values ("misspecified" parameters) than those used to generate the optimal designs.
- Step 5 - Statistical Comparison: Compute an empirical D-criterion confidence interval (using bootstrap methods on the simulation results) for each design to allow for objective statistical comparison.
5. Key Outputs & Metrics:
- Number of optimal support points.
- Bias of parameter estimates.
- Empirical D-criterion value and its confidence interval.
- Comparison of predicted vs. empirical standard errors.
Diagram 2: Performance Evaluation Workflow for FIM Designs (77 chars)
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Software Tools for FIM-Based Optimal Design
| Software Tool | Primary Function | Key Feature for FIM Research |
|---|---|---|
| PFIM | Design evaluation & optimization | Implements both Full and Block-Diagonal FIM approximations for population models [44]. |
| PopED (Pop. Exp. Designer) | Design optimization & exploration | Flexible platform for comparing D-optimal designs using different FIM approximations and constraints. |
| POPT | Optimal design computation | Used in comparative studies to benchmark FIM performance [44]. |
| NONMEM/PsN | PK/PD Modeling & Simulation | Industry standard for running the Monte Carlo Simulation and Estimation (MCSE) studies needed to empirically validate FIM-optimal designs [8]. |
R/Shiny Apps (e.g., PFIMx) |
Interactive design interface | Provides accessible graphical interfaces for implementing advanced FIM calculations. |
Table 4: Conceptual & Mathematical "Reagents"
| Concept/Tool | Description | Role in FIM Implementation |
|---|---|---|
| FO Approximation | Linearizes random effects around their mean (zero). | Faster FIM calculation; can increase clustering and bias [8]. |
| FOCE Approximation | Linearizes around conditional estimates of random effects. | More accurate for nonlinear models; used with Full FIM to reduce clustering [8]. |
| D-Optimality Criterion | Maximizes the determinant of the FIM. | The objective function used to find designs that minimize overall parameter uncertainty [8]. |
| Monte Carlo Simulation & Estimation (MCSE) | Gold-standard evaluation via synthetic data. | Provides empirical performance metrics (bias, SE) to validate and compare FIM-based designs [8] [44]. |
| Bootstrap Confidence Intervals | Statistical resampling technique. | Used to quantify uncertainty in the empirical D-criterion, allowing statistical comparison of designs [8]. |
Frequently Asked Questions (FAQs): Foundational Concepts
Q1: What is parameter or model misspecification in the context of drug development experiments? Model misspecification occurs when the mathematical or statistical model used to design an experiment or analyze data does not perfectly represent the true underlying biological or chemical process [45]. In drug development, this is common because simple, interpretable models (e.g., the Emax model for dose-response) are used to approximate highly complex systems. The discrepancy between the simple model and reality can lead to biased estimates, incorrect conclusions, and failed experiments if not accounted for [45].
Q2: How does the Fisher Information Matrix (FIM) relate to managing uncertainty in experiments? The Fisher Information Matrix (FIM) is a foundational mathematical construct that quantifies the amount of information an observable data set carries about the unknown parameters of a model [30]. Its inverse sets a lower bound (the Cramér–Rao bound) on the variance of any unbiased parameter estimator. In optimal experimental design (OED), the FIM is used as an objective function to be maximized, guiding the selection of experimental conditions (e.g., dose levels, sampling times) that minimize the expected parameter uncertainty [30].
Q3: Why do classical optimal designs fail under model misspecification, and what is the modern robust approach? Classical OED theory typically assumes the model is correct. Under this assumption, the optimal design does not depend on the sample size [45]. However, when the model is misspecified, this approach can lead to designs that perform poorly because they may over-explore regions of the design space that are only informative for the wrong model. Modern robust approaches explicitly incorporate the possibility of misspecification. One advanced method treats the misspecification as a stochastic process (a random effect) added to the simple parametric model (the fixed effect). The design is then optimized to efficiently estimate this combined "true" mean function, leading to designs that adapt based on available sample size and expected model error [45].
Q4: What are the key regulatory phases of clinical drug development, and how does uncertainty change across them? Clinical investigation of a new drug proceeds through phased studies under an Investigational New Drug (IND) application [46]. Table: Phases of Clinical Drug Development [46]
| Phase | Primary Goal | Typical Subject Count | Key Information Gathered |
|---|---|---|---|
| Phase 1 | Initial safety, pharmacokinetics, pharmacodynamics | 20-80 healthy volunteers | Metabolic profile, safe dosage range, early evidence of activity. |
| Phase 2 | Preliminary efficacy, short-term safety in patients | Several hundred patients | Effectiveness for a specific indication, common side effects. |
| Phase 3 | Confirmatory evidence of efficacy, safety profile | Several hundred to several thousand patients | Comprehensive benefit-risk relationship, basis for labeling. |
Uncertainty is highest in Phase 1, where prior human data is limited. As development progresses, the increasing sample size and evolving knowledge should inform more robust, adaptive designs that account for earlier model inaccuracies [46] [45].
Q5: What advanced computational methods help manage misspecification in complex, simulation-based models? For complex mechanistic models where the likelihood function is intractable but simulation is possible, Simulation-Based Inference (SBI) techniques like Sequential Neural Likelihood (SNL) are used. Standard SNL can produce overconfident and inaccurate inferences under model misspecification. Cutting-edge methods introduce adjustment parameters to the model, allowing it to detect and correct for systematic discrepancies between simulator outputs and observed data. This provides more accurate parameter estimates and reliable uncertainty quantification even when the core model is imperfect [47].
Technical Troubleshooting Guides
Troubleshooting Assay Performance & Data Quality
Issue: Poor or No Assay Window in TR-FRET or Fluorescence-Based Assays.
- Symptoms: Low signal-to-noise, inability to distinguish between positive and negative controls, failed Z'-factor calculation.
- Diagnosis & Resolution Protocol:
- Confirm Instrument Setup: The most common cause is incorrect instrument configuration. Verify that the exact recommended emission and excitation filters for your assay and instrument model are installed [48].
- Validate Reagent Integrity: Ensure reagents are stored correctly, have not expired, and were prepared according to the Certificate of Analysis (CoA). Test the instrument setup using control reagents from your assay kit [48].
- Check Liquid Handling: For assays using nanoliter dispensers (e.g., I.DOT):
- Perform a DropDetection validation. Clean the detection board with 70% ethanol and run a test protocol with water [49].
- Ensure the dispense head is correctly aligned and sealed, and there is no pressure leakage [49].
- Verify that the correct liquid class is assigned for the specific source plate and solvent (e.g., DMSO) you are using, as this controls droplet formation physics [49].
- Eliminate Contamination: For ultra-sensitive assays (e.g., HCP ELISAs), contamination from concentrated analyte sources (e.g., serum, cell culture media) is a major risk. Perform assays in a clean, dedicated space, use aerosol barrier pipette tips, and do not breathe or talk over uncovered plates [50].
Issue: Inconsistent EC50/IC50 Values Between Replicates or Labs.
- Symptoms: High variability in potency estimates for the same compound, poor reproducibility.
- Diagnosis & Resolution Protocol:
- Standardize Stock Solutions: The primary reason for inter-lab differences is variation in compound stock solution preparation (typically at 1 mM). Implement standardized protocols for weighing, solubilization (e.g., in DMSO), and storage [48].
- Employ Ratiometric Data Analysis: For TR-FRET assays, always use the emission ratio (Acceptor RFU / Donor RFU) rather than raw acceptor signal. The donor signal acts as an internal reference, normalizing for pipetting errors and lot-to-lot reagent variability [48].
- Use Appropriate Curve Fitting: Avoid forcing data into a linear regression model. Immunoassay and potency data are often inherently non-linear. Use robust fitting routines like 4-parameter logistic (4PL), point-to-point, or cubic spline for accurate interpolation, especially at the curve extremes [50].
- Assess Data Quality with Z'-Factor: The assay window alone is insufficient. Calculate the Z'-factor, which incorporates both the signal dynamic range and the data variability. An assay with a Z'-factor > 0.5 is generally considered suitable for screening [48].
- Formula:
Z' = 1 - [ (3σ_positive + 3σ_negative) / |μ_positive - μ_negative| ] - Interpretation: A value of 0.5 means 50% of the separation between control means is free of noise overlap.
- Formula:
Issue: High Background or Non-Specific Binding (NSB) in ELISA.
- Symptoms: Abnormally high absorbance in the zero standard or blank wells, reducing assay sensitivity.
- Diagnosis & Resolution Protocol:
- Optimize Washing: Incomplete washing is a frequent cause. Follow the kit's washing procedure precisely. Do not over-wash or let wash buffer soak, as this can reduce specific binding [50].
- Check Reagent Contamination: Ensure substrate solutions (e.g., PNPP for alkaline phosphatase) are not contaminated. Aliquot substrate and avoid returning unused portions to the stock bottle [50].
- Validate Diluents: If diluting samples, use the kit-specific diluent or rigorously validate an in-house diluent with a spike-and-recovery experiment (target: 95-105% recovery) [50].
Troubleshooting Optimal Design Implementation
Issue: Optimal Design Seems Overly Sensitive to Initial Parameter Guesses.
- Symptom: Small changes in the prior parameter estimates lead to vastly different suggested experimental designs.
- Resolution Strategy: Move from local optimality (which depends on a single best parameter guess) to Bayesian or robust optimality. Instead of a single FIM, optimize the expectation of your design criterion (like the determinant of the FIM, D-optimality) over a prior distribution of the parameters. This produces designs that perform well on average across the range of plausible parameter values [51] [52].
Issue: Experimental Results Consistently Deviate from Model Predictions, Causing Failed Go/No-Go Decisions.
- Symptom: Systematic model discrepancy invalidates inferences.
- Resolution Strategy: Implement a misspecification-robust design framework.
- Formalize the Discrepancy: Explicitly model the misspecification term,
C(x), as a stochastic process (e.g., a Gaussian process) added to your core scientific model,ν(x)[45]. The combined model isμ(x) = ν(x) + C(x). - Re-define the Objective: Design experiments not just to estimate parameters of
ν(x), but to best predict the overall response surfaceμ(x). This often involves optimizing a modified information matrix that accounts for the covariance structure ofC(x)[45]. - Iterate and Learn: Use early-phase data to characterize the discrepancy
C(x). Update the model and the design for subsequent phases adaptively, focusing resources on regions critical for decision-making [45] [52].
- Formalize the Discrepancy: Explicitly model the misspecification term,
Experimental Protocols for Robust Design
Protocol: Robust Optimal Design for a Dose-Response Study
Objective: To design a Phase 2 dose-ranging study that provides efficient estimates of the Emax model parameters while remaining robust to potential model misspecification.
Theoretical Foundation: This protocol implements a unified approach where the true mean response μ(x) is the sum of a parsimonious 4-parameter Emax model (ν(x)) and a non-parametric misspecification process (C(x)), modeled as a zero-mean Gaussian process with a specified kernel [45].
Materials: See "The Scientist's Toolkit" below. Pre-Experimental Software Setup:
- Specify the design space
X(e.g., 5-6 plausible dose levels within a safe range). - Define the fixed-effect model
ν(x)(the Emax function). - Specify the covariance kernel for the Gaussian process
C(x)(e.g., squared-exponential). The length-scale of this kernel encodes beliefs about the smoothness of the model error. - Specify prior distributions for the Emax parameters (e.g., ED50, Hill coefficient) based on preclinical or Phase 1 data.
- Choose a robust optimality criterion, such as maximizing the expectation (over the prior) of the log determinant of the total information matrix for predicting
μ(x).
Computational Design Generation:
- Use an optimization algorithm (e.g., Fedorov's exchange algorithm, particle swarm) to allocate a fixed number of patient cohorts
Nacross the doses inX. - The algorithm will evaluate the robust criterion for each candidate design, factoring in both the information from the parametric model and the uncertainty from the misspecification term.
- Expected Outcome: With small
N, the optimal design will resemble a classical D-optimal design for the Emax model. AsNincreases, the design will strategically place more observations at doses where the model's predictive uncertainty due to potential misspecification is highest, often near the ED50 or other critical decision points [45].
Diagram: Workflow for Robust Optimal Experimental Design
Protocol: Validating Assay Robustness with Z'-Factor and Signal Ratio Analysis
Objective: To empirically verify that an assay system is producing reliable, high-quality data suitable for screening or parameter estimation, independent of absolute instrument signal values.
Background: The Z'-factor integrates both the assay window (separation between controls) and the data variability, providing a single metric for assay quality [48]. Ratiometric analysis (e.g., in TR-FRET) controls for technical noise [48].
Procedure:
- Prepare Control Plates: On at least three independent plates, run the assay using high (positive) and low (negative) control conditions, with a minimum of 12 replicates each.
- Collect Raw Data: For each well, record the raw signals for both channels (e.g., Donor at 495 nm and Acceptor at 520 nm for Tb assays).
- Calculate Emission Ratios: For each well, compute the ratio
R = Acceptor RFU / Donor RFU[48]. - Compute Statistics: For the positive (
pos) and negative (neg) control groups, calculate the mean (μ_pos,μ_neg) and standard deviation (σ_pos,σ_neg) of the ratiosR. - Calculate Z'-Factor: Apply the formula:
Z' = 1 - [ 3*(σ_pos + σ_neg) / |μ_pos - μ_neg| ]. - Interpretation: A
Z' > 0.5indicates an excellent assay suitable for screening. AZ'between0and0.5is marginal but may be usable. AZ' < 0indicates the assay is not reliable [48].
Troubleshooting Step: If the Z'-factor is low, investigate the cause using the ratio data:
* High variability (σ): Indicates pipetting errors, contamination, or instrument instability.
* Small assay window (|μ_pos - μ_neg|): Indicates incorrect controls, inactive reagents, or instrument filter/setup issues [48].
The Scientist's Toolkit: Key Reagents & Materials
Table: Essential Research Reagents and Solutions for Robust Experimentation
| Item | Function & Role in Managing Uncertainty | Key Consideration for Robustness |
|---|---|---|
| Validated Assay Kits (e.g., TR-FRET Kinase Assay) | Provide standardized, optimized reagents for measuring specific biochemical activities (e.g., phosphorylation). Reduce inter-experiment variability. | Lot-to-lot consistency is critical. Always perform ratiometric analysis (Acceptor/Donor) to normalize for minor lot variations [48]. |
| Reference Standards & Controls | Used to calibrate assays, define the assay window, and calculate the Z'-factor for quality control. Anchor data in a reproducible metric. | Use stable, well-characterized materials. Include both positive and negative controls in every run to continuously monitor assay performance [48]. |
| Precision Liquid Handlers (e.g., I.DOT) | Enable accurate, nanoliter-scale dispensing for dose-response curves and assay miniaturization. Reduce reagent costs and increase throughput. | Correct Liquid Class selection is paramount for droplet formation accuracy. Must be validated for each solvent type (e.g., DMSO vs. water) [49]. |
| Kit-Specific Assay Diluent | The matrix used to dilute samples and standards. Maintains constant background and prevents non-specific interference. | Using the kit-provided diluent ensures your sample matrix matches the standard curve matrix, preventing dilution-induced artifacts and ensuring accurate recovery [50]. |
| High-Sensitivity ELISA Reagents | Detect low-abundance impurities like Host Cell Proteins (HCPs). Essential for process-related safety assays. | Prone to contamination. Must use strict contamination control protocols: dedicated space, aerosol barrier tips, careful handling of substrates [50]. |
| Model Misspecification Term (C(x)) | A statistical construct (e.g., Gaussian Process) representing the unknown discrepancy between the simple model and reality. | The choice of covariance kernel (e.g., squared-exponential, Matérn) encodes assumptions about the smoothness and scale of the model error, influencing the robust design [45]. |
Core Theoretical Framework & Visualization
The core advancement in managing misspecification is the shift from a purely parametric to a semi-parametric or Bayesian nonparametric framework for design.
Diagram: Relationship Between True Process, Models, and Robust Design
The Workflow Logic:
- The researcher posits a Simple Model
ν(x)based on scientific knowledge (e.g., Michaelis-Menten kinetics) [45]. - Acknowledging its inevitable imperfection, a Misspecification Term
C(x)is formally included. This term is not a mere error but a structured random function representing unknown model deviation [45]. - The Combined Model
μ(x)becomes the target for inference and prediction. - A Robust Optimal Design is computed to maximize the information gained about
μ(x). This design depends on sample size: with little data, it trustsν(x)more; with abundant data, it invests in learningC(x)[45] [51]. - Data collected under this design is used to estimate the full combined model, yielding parameters for
ν(x)and a realization ofC(x). - The estimated discrepancy informs model refinement and future designs, closing the iterative "Box Loop" of scientific learning [47].
Technical Support Center: Optimal Experimental Design
Welcome to the Technical Support Center for Optimal Experimental Design (OED). This resource provides targeted troubleshooting guides and FAQs for researchers implementing advanced design strategies in pharmacometrics, drug development, and related fields. The content is framed within the broader thesis of Fisher Information Matrix (FIM) research, focusing on practical solutions for challenges in clustering, support point identification, and computational efficiency [8] [53].
In nonlinear mixed-effects models (NLMEMs), the Fisher Information Matrix (FIM) quantifies the information an experimental design provides about unknown model parameters [2]. Optimizing the design by maximizing a scalar function of the FIM (e.g., D-optimality) leads to more precise parameter estimates and more informative studies [8]. Key challenges in this process include:
- Clustering: The tendency for optimal sampling times to cluster at a few distinct time points (support points), which may reduce robustness if model assumptions are wrong [8].
- Support Points: The specific time points in an optimal design where samples should be taken. The number and location of these points are critical for design efficiency [53].
- Computational Efficiency: Calculating and optimizing the
FIMfor NLMEMs is complex and requires approximations (like FO or FOCE), which impact the resulting design and computational cost [8].
Troubleshooting Guides
Issue 1: High Parameter Bias or Unrealistic Clustering in D-Optimal Design
Problem: Your D-optimal design produces extreme clustering of samples at very few time points, or subsequent simulation-estimation reveals high bias in parameter estimates.
- Potential Cause 1: Using the FO Approximation with a Block-Diagonal FIM. The First Order (
FO) approximation, combined with a block-diagonalFIMimplementation that assumes independence between fixed and random effects, can lead to designs with fewer support points and excessive clustering. This design may be sensitive to parameter misspecification [8].- Solution: Switch to the First Order Conditional Estimation (
FOCE) approximation and a fullFIMimplementation. Research shows this combination yields designs with more support points and less clustering, which often provides greater robustness to errors in initial parameter estimates [8].
- Solution: Switch to the First Order Conditional Estimation (
- Potential Cause 2: Severe Misspecification of Initial Parameters. The optimal design for a nonlinear model depends on the initial parameter values (
θ). A poor initial guess can lead to a locally optimal design that performs poorly under the true parameters [53].- Solution:
- Perform a robustness or sensitivity analysis. Re-optimize the design across a plausible range of parameter values derived from literature or a pilot study.
- Implement a sequential design strategy. Start with an initial design based on the best available guesses, collect a portion of the data, re-estimate parameters, and then re-optimize the design for the remaining experimental runs [53].
- Consider a global clustering approach. Sample different possible parameter values (e.g., via Monte Carlo), compute the optimal design for each, and then cluster the resulting support points to find regions in the design space that are frequently optimal [53].
- Solution:
Issue 2: Excessive Computation Time for FIM Evaluation and Design Optimization
Problem: The process of calculating the FIM and optimizing the design is prohibitively slow, hindering iterative development or robust design strategies.
- Potential Cause 1: Using the FOCE Approximation for Exploratory Optimization. While more accurate, the
FOCEapproximation is significantly more computationally intensive thanFOas it requires linearization around individual samples of the random effects [8].- Solution: Adopt a multi-fidelity approach. Use the faster
FOapproximation for initial exploratory optimization and robustness tests. Switch to theFOCEapproximation only for the final design refinement to ensure accuracy [8].
- Solution: Adopt a multi-fidelity approach. Use the faster
- Potential Cause 2: Optimizing Over a Dense, Unstructured Grid of Possible Time Points. Evaluating the
FIMat every point in a fine grid of candidate times is wasteful.- Solution: Use an adaptive grid or candidate set reduction. Begin optimization with a coarse grid. After identifying promising regions (potential support points), refine the grid selectively around these areas in subsequent iterations. Algorithms like the Vertex Exchange Method (
VEM) or Weighted-Discretization-Approach are designed for this efficiency [53].
- Solution: Use an adaptive grid or candidate set reduction. Begin optimization with a coarse grid. After identifying promising regions (potential support points), refine the grid selectively around these areas in subsequent iterations. Algorithms like the Vertex Exchange Method (
- Potential Cause 3: Direct Optimization of High-Dimensional Molecular Descriptors in Cheminformatics. Clustering large libraries of small molecules using all available high-dimensional features (e.g., thousands of molecular descriptors) is slow [54].
- Solution: Apply dimensionality reduction as a pre-processing step. Use techniques like Principal Component Analysis (
PCA) or Uniform Manifold Approximation and Projection (UMAP) to project the data into a lower-dimensional space where distance calculations are cheaper, before performing clustering [54].
- Solution: Apply dimensionality reduction as a pre-processing step. Use techniques like Principal Component Analysis (
Issue 3: Poor Quality or Uninterpretable Clustering of Chemical Data
Problem: The clusters of small molecules from a virtual screening library do not seem chemically meaningful, or the clustering algorithm gives inconsistent results.
- Potential Cause 1: Choice of Clustering Algorithm and Metrics. Different algorithms (hierarchical vs. non-hierarchical) and distance metrics (Tanimoto, Euclidean) produce different cluster structures. The "ground truth" for chemical clustering is often subjective and goal-dependent [54].
- Solution:
- Define the goal clearly. Are you maximizing chemical diversity for a broad screen or focusing on a specific chemotype? This guides algorithm choice [54].
- Use quantitative validation metrics. Do not rely solely on visual inspection. Calculate the silhouette coefficient (measures cluster cohesion and separation) or the Calinski-Harabasz score to assess clustering quality objectively [54].
- Experiment with subspace or multi-view clustering. If molecules can be grouped differently based on different features (e.g., shape vs. pharmacophores), these advanced methods can provide a more nuanced view [54].
- Solution:
- Potential Cause 2: Noisy or Poorly Selected Molecular Features. The input feature vector does not adequately capture the relevant chemical or biological properties for your task.
- Solution: Curate the feature set. Use domain knowledge or feature selection algorithms to identify and use the most relevant molecular descriptors. Consider using learned feature representations from autoencoders, as in the
DeepClusteringtool [54].
- Solution: Curate the feature set. Use domain knowledge or feature selection algorithms to identify and use the most relevant molecular descriptors. Consider using learned feature representations from autoencoders, as in the
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between the full FIM and the block-diagonal FIM, and why does it matter?
A1: The full FIM accounts for potential correlations between all estimated parameters, including both fixed effects (β) and variance components (ω², σ²). The block-diagonal FIM makes a simplifying assumption that the fixed effects are independent of the random effect variances, setting the cross-derivative terms between them to zero [8]. This approximation reduces computational complexity but can lead to different optimal designs, typically with more clustered support points, which may be less robust [8].
Q2: My optimal design software allows for "support points." What are these, and how many should I expect?
A2: Support points are the distinct time points (or design variable levels) in an optimal design where measurements are scheduled. For a model with p parameters, the number of support points in a locally D-optimal design can be as low as p, but often more are found, especially with complex models and sufficient allowable samples per subject [8]. The FOCE approximation with the full FIM generally produces designs with more support points than the FO/block-diagonal combination [8].
Q3: How can I assess the performance of my optimal design before running the actual experiment? A3: The gold standard is a Monte Carlo Simulation-Estimation (MCSE) study.
- Simulate: Use your proposed design and the assumed model to generate hundreds or thousands of synthetic datasets.
- Estimate: Fit the model to each synthetic dataset.
- Evaluate: Calculate the empirical bias and precision (coefficient of variation) of the parameter estimates across all runs. Compare these metrics to your target values (e.g., bias < 10%, precision < 30%). This method objectively evaluates design performance beyond just the
FIM-based optimality criterion [8].
Q4: For clustering small molecules from a large library, how do I choose the right number of clusters (k)? A4: There is no single correct answer, but systematic methods exist. A common approach is the elbow method:
- Run the clustering algorithm (e.g., k-means) for a range of
kvalues. - For each
k, calculate a measure of clustering "goodness" (e.g., within-cluster sum of squares). - Plot this measure against
k. Look for the "elbow" – the point where the rate of improvement sharply decreases. Thiskoften provides a good balance between detail and generalization [54]. Always complement this with domain expertise.
Q5: What are some freely available software tools for implementing these advanced design and clustering methods? A5: Several open-source and freely accessible tools are available, as summarized in the table below.
Table 1: Research Reagent Solutions – Key Software Tools
| Tool Name | Primary Function | Brief Description & Utility |
|---|---|---|
| PopED | Optimal Experimental Design | Software for population optimal design in NLMEMs. Supports FO/FOCE approximations and various FIM calculations [8]. |
| PFIM | Optimal Experimental Design | A widely used tool for evaluating and optimizing population designs for pharmacokinetic-pharmacodynamic (PKPD) models [8]. |
| RDKit & ChemmineR | Cheminformatics & Clustering | Open-source cheminformatics toolkits. Provide functions for handling chemical data, computing descriptors, and performing clustering (e.g., Butina clustering) [54]. |
| UMAP | Dimensionality Reduction | A robust technique for reducing high-dimensional data (like molecular descriptors) to 2D or 3D for visualization and more efficient subsequent clustering [54]. |
| DeepClustering | Advanced Molecular Clustering | An open-source approach that uses deep learning (autoencoders) for dimensionality reduction before clustering, capturing complex patterns in molecular data [54]. |
Experimental Protocols
Protocol 1: Robust Optimal Design via Parameter Uncertainty Sampling
This protocol creates a design robust to parameter uncertainty using a global clustering approach [53].
Objective: To generate an optimal sampling schedule that performs well over a distribution of possible parameter values.
Materials: Pharmacometric model, software capable of FIM calculation and optimization (e.g., PopED), prior distributions for model parameters.
Method:
- Define Uncertainty: Specify plausible prior distributions (e.g., multivariate normal) for the model parameters (
θ) based on literature or pilot data. - Sample Parameters: Draw
N(e.g., 1000) parameter vectors from the prior distributions. - Compute Local Designs: For each sampled parameter vector
θ_i, compute the locally D-optimal design (set of support points and weights). - Cluster Support Points: Pool all support points from all
Nlocal designs. Use a spatial clustering algorithm (e.g., k-means or DBSCAN) on the time-point coordinate to identifyMdense regions in the design space. - Form Robust Design: Select the centroid of each of the
Mclusters as a final support point. Assign weights proportional to the frequency of points in each cluster. - Validate: Perform an MCSE study comparing this robust design to a standard locally optimal design under various true parameter conditions.
Protocol 2: Evaluating FIM Approximation Impact on Design Performance
This protocol quantifies how the choice of FIM approximation (FO vs. FOCE, full vs. block-diagonal) affects final design quality [8].
Objective: To select the most appropriate FIM approximation method for a specific PK/PD model.
Materials: A candidate NLMEM, true or best-guess parameters, optimal design software.
Method:
- Generate Competing Designs: Using the same model and parameters, optimize the sampling schedule four separate times, creating:
- Design A:
FOapproximation + Block-diagonalFIM - Design B:
FOapproximation + FullFIM - Design C:
FOCEapproximation + Block-diagonalFIM - Design D:
FOCEapproximation + FullFIM
- Design A:
- Record Design Characteristics: For each design, note the number of unique support points and the degree of clustering.
- Perform MCSE Evaluation:
- Simulate 500 datasets for each design under the assumed (true) parameters.
- Fit the model to each dataset.
- Compute the empirical bias and precision for key parameters.
- (Optional) Repeat simulation with misspecified parameters to test robustness.
- Analyze: Compare the bias/precision metrics across designs. The design with the lowest bias and adequate precision, balanced against its computational cost, is recommended.
Visualizations
Diagram 1: Optimal Design Workflow with Clustering for Robustness
Workflow for a Robust Optimal Experimental Design
Diagram 2: FIM Approximation Impact on Design & Performance
How FIM Approximation Choices Influence Design Outcomes
Ensuring Success: How to Validate and Compare Your Optimal Designs
Technical Support Center: Troubleshooting FIM-Based Optimal Experimental Design
This technical support center provides resources for researchers, scientists, and drug development professionals working within the context of optimal experimental design (OED) and Fisher Information Matrix (FIM) research. The following guides and FAQs address common practical challenges and theoretical limitations encountered when applying asymptotic, FIM-based criteria to design real-world experiments, particularly in pharmacometrics and systems biology.
Frequently Asked Questions (FAQs)
Q1: When do standard FIM-based optimality criteria fail or become unreliable? Standard FIM-based criteria rely on asymptotic theory and several key assumptions that often break down in practice, leading to unreliable designs [3]. The primary failure modes occur when the underlying statistical model cannot be adequately linearized or when data distributions violate Gaussian assumptions [55] [8]. In nonlinear mixed-effects models (NLMEMs) common in pharmacometrics, the exact FIM is analytically intractable and must be approximated (e.g., using First Order (FO) or First Order Conditional Estimation (FOCE) methods) [43] [8]. These approximations perform poorly when inter-individual variability is high, model nonlinearity is strong, or when parameters are misspecified during the design phase [8]. Furthermore, for discrete data (e.g., single-cell expression counts) or data with complex, non-Gaussian distributions, standard FIM formulations that assume continuous, normally distributed observables can severely misrepresent the actual information content [55] [56].
Q2: My optimal design, based on maximizing the D-criterion, resulted in highly clustered sampling points. Is this a problem? Yes, clustered sampling points can be a significant vulnerability. D-optimal designs that maximize the determinant of the FIM often cluster samples at a few specific, parameter-dependent support points [8]. While theoretically efficient if the model and its parameters are perfectly known, this clustering reduces robustness. In practice, models are approximations and true parameters are unknown. If the assumed parameter values are misspecified during the design calculation, the clustering will occur at suboptimal points, potentially degrading the quality of parameter estimation [8]. Designs with more support points (achieved, for example, by using the FOCE approximation and a Full FIM implementation) tend to be more robust to such parameter misspecification [43] [8].
Q3: How can I design experiments for systems with discrete, non-Gaussian outcomes (e.g., low molecule counts in single-cell biology)? Standard FIM approaches are insufficient for discrete stochastic systems. You should use methods specifically developed for the chemical master equation (CME) framework, such as the Finite State Projection-based FIM (FSP-FIM) [55]. The FSP-FIM uses the full probability distribution of molecule counts over time, making no assumptions about the distribution shape (e.g., Gaussian). This allows for the optimal design of experiments (like timing perturbations or measurements) that account for intrinsic noise and complex distributions, which are common in gene expression data [55]. This method is a key advancement for co-designing quantitative models and single-cell experiments.
Q4: How do I accurately compute the FIM for discrete mixed-effects models (e.g., count or binary data in clinical trials)? For discrete mixed-effects models (generalized linear or nonlinear), the likelihood lacks a closed form, making FIM computation challenging [56]. A recommended method is the Monte Carlo/Adaptive Gaussian Quadrature (MC/AGQ) approach [56]. Unlike methods based on marginal quasi-likelihood (MQL) approximation, the MC/AGQ method is based on derivatives of the exact conditional likelihood. It uses Monte Carlo sampling over random effects and adaptive Gaussian quadrature for numerical integration, providing a more accurate FIM approximation, especially for variance parameters [56]. This allows for better prediction of parameter uncertainty (Relative Standard Error) and power calculations for detecting covariate effects [14] [56].
Q5: What is the practical difference between using a "Full FIM" and a "Block-Diagonal FIM" implementation in design software? The choice impacts design robustness. The Full FIM accounts for interactions between fixed effect parameters (e.g., drug clearance) and variance parameters (e.g., inter-individual variability) [8]. The Block-Diagonal FIM assumes these sets of parameters are independent, simplifying calculation [43]. Research indicates that using the Full FIM implementation, particularly with the FOCE approximation, generates designs with more support points and less clustering [8]. These designs have demonstrated superior performance when evaluated under conditions of parameter misspecification, making them more reliable for real-world application where true parameters are unknown [43] [8].
Q6: The Cramér-Rao Lower Bound (CRLB) derived from the FIM seems very optimistic compared to my simulation results. Why?
This is a common issue highlighting the limits of asymptotic evaluation. The CRLB (Var(θ̂) ≥ I(θ)⁻¹) is an asymptotic lower bound for the variance of an unbiased estimator [2] [3]. Its accuracy depends on several conditions: a correctly specified model, unbiased and efficient (e.g., maximum likelihood) estimation, and a sufficiently large sample size for asymptotic theory to hold [3]. In pharmacometrics, sample sizes (number of individuals) are often limited. Furthermore, the FIM itself is usually an approximation (FO/FOCE), and model misspecification is common. Therefore, the CRLB often represents an unattainable ideal. Always validate your optimal design using clinical trial simulation (CTS), which involves repeatedly simulating data from your model, re-estimating parameters, and examining the empirical covariance matrix. This provides a realistic assessment of expected parameter precision [56] [8].
Troubleshooting Guides
Issue 1: High Predicted vs. Empirical Parameter Uncertainty
Problem: Parameter uncertainties (Relative Standard Errors) predicted from the inverse FIM are much smaller than those obtained from clinical trial simulation (CTS). Diagnosis & Solution: This typically indicates a breakdown of asymptotic assumptions.
- Verify FIM Approximation: If using an FO approximation for an NLMEM, switch to a more accurate FOCE or Monte Carlo-based FIM calculation [43] [56]. The FO approximation can be poor with high inter-individual variability.
- Check Sample Size: The CRLB is an asymptotic result. With a small number of individuals (N), the empirical uncertainty will be larger. Use CTS, not just the FIM, to evaluate feasibility for your specific N [3].
- Review Model Nonlinearity: Strong nonlinearity in the parameters can make the likelihood function non-quadratic, violating local asymptotic assumptions. Consider a robust design criterion or a design that spreads support points.
Issue 2: Optimal Design is Logistically or Ethically Infeasible
Problem: The algorithm suggests sampling schedules with too many samples, samples at impractical times, or extreme dose levels. Diagnosis & Solution: The D-optimal criterion is "greedy" for information and ignores practical constraints.
- Formalize Constraints: Explicitly encode constraints into the optimization problem: minimum time between samples, fixed time windows (e.g., clinic hours), maximum total blood volume, safe dose ranges [3].
- Use a Constrained Optimization Algorithm: Employ algorithms that can handle nonlinear constraints (e.g., sequential quadratic programming) instead of unconstrained optimization.
- Explore Alternative Criteria: Consider a robust (e.g., maximin) or a Bayesian optimal design that accounts for parameter uncertainty, which may yield more balanced, implementable designs.
Issue 3: Failure to Detect a Covariate Effect
Problem: A post-hoc analysis finds no significant covariate effect, but the FIM-based power analysis predicted high power to detect it. Diagnosis & Solution: The power prediction was likely based on an inaccurate FIM or incorrect assumptions.
- Audit the FIM for Covariate Parameters: Ensure the FIM calculation correctly includes the covariate model. Methods exist to compute the FIM's expectation over the joint distribution of covariates (discrete and continuous) to predict uncertainty and power for covariate effects [14].
- Validate with Simulation (CTS for Power): Never rely solely on FIM-based power. Perform a full power analysis via simulation: simulate hundreds of datasets under the alternative hypothesis (i.e., with the covariate effect present), analyze each one, and compute the proportion of times the effect is found significant [14] [56]. This is the gold standard.
- Check Covariate Distribution: The assumed distribution of the covariate in the design phase may not match the real enrollment population, affecting power.
Key Experimental Protocols & Data Analysis Workflows
Protocol 1: Implementing the Monte Carlo/AGQ Method for Exact FIM Computation
Application: Accurate FIM evaluation for discrete-response mixed-effects models (GLMMs/NLMEMs) for optimal design [56]. Methodology:
- Define the Conditional Likelihood: Specify the probability model
P(Y_i | η_i, ξ_i)for individuali's dataY_i, given random effectsη_iand designξ_i. - Compute Derivatives: Analytically or automatically differentiate the log of the conditional likelihood with respect to all parameters
θ(fixed effects and variances). - Monte Carlo Integration over Random Effects: For each individual, take
Ssamples (η_i^(s)) from the distribution of random effectsN(0, Ω). - Adaptive Gaussian Quadrature (AGQ): For each Monte Carlo sample
η_i^(s), use AGQ (withQnodes) to numerically compute the integral over the conditional likelihood derivatives. AGQ adapts the quadrature nodes to the location and scale of the integrand, improving accuracy over standard quadrature. - Average and Sum: Average the results over the
SMonte Carlo samples for an individual, then sum over allNindividuals to form the expected FIM.
Workflow Diagram:
Diagram: Workflow for MC/AGQ FIM Computation [56].
Protocol 2: Finite State Projection FIM (FSP-FIM) for Single-Cell Experiment Design
Application: Designing optimal perturbation/measurement experiments for stochastic gene expression models with discrete, non-Gaussian data [55]. Methodology:
- Formulate the Chemical Master Equation (CME): Define the model states (e.g., mRNA/protein counts) and reaction propensities.
- Apply the Finite State Projection (FSP): Truncate the infinite state space to a finite set
X_Jthat contains most of the probability mass, converting the CME into a finite linear systemdp/dt = A p. The error is computable and bounded [55]. - Compute Likelihood & Sensitivity: For a candidate experiment design (e.g., measurement time
t), compute the solutionp(t; θ). The likelihood for single-cell snapshot data is multinomial. Use the FSP to also compute the parameter sensitivity∂p/∂θ. - Calculate the FSP-FIM: Compute
FIM(θ) = (∂p/∂θ)^T * diag(1/p) * (∂p/∂θ)(for multinomial observations). This uses the full distributionp, not just its moments. - Optimize Design: Use the FSP-FIM in a standard optimal design criterion (e.g., D-optimal) to select design variables (e.g., time points) that maximize information gain about parameters
θ.
Table 1: Impact of FIM Approximation and Implementation on Optimal Design Robustness [43] [8]
| FIM Approximation | FIM Implementation | Typical Design Characteristic | Robustness to Parameter Misspecification | Computational Cost |
|---|---|---|---|---|
| First Order (FO) | Block-Diagonal | Fewer support points; high clustering of samples | Low (Higher bias) [8] | Low |
| First Order (FO) | Full | Intermediate support points | Intermediate | Medium |
| First Order Conditional Estimation (FOCE) | Block-Diagonal | More support points than FO | Medium | High |
| First Order Conditional Estimation (FOCE) | Full | Most support points; least clustering | High (Recommended for robustness) [43] [8] | Highest |
Table 2: Comparison of FIM Computation Methods for Non-Standard Data [55] [56]
| Method | Best For | Key Principle | Advantage | Limitation |
|---|---|---|---|---|
| Linear Noise Approximation FIM (LNA-FIM) | High molecule count systems | Approximates distribution as Gaussian via linearization of noise. | Simple, fast. | Inaccurate for low counts/high noise [55]. |
| Sample Moments FIM (SM-FIM) | Large # of cells (flow cytometry) | Uses Central Limit Theorem on sample mean/covariance. | Works for large cell populations. | Poor for small samples or long-tailed distributions [55]. |
| Finite State Projection FIM (FSP-FIM) | Single-cell data with intrinsic noise | Uses full discrete distribution from Chemical Master Equation. | Exact for truncated system; handles any distribution shape [55]. | State space can grow large. |
| Monte Carlo/AGQ FIM | Discrete mixed-effects models | Uses exact conditional likelihood + numerical integration. | More accurate than MQL/PQL, especially for variances [56]. | Computationally intensive. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational and Experimental Reagents for Advanced FIM-Based Design
| Item / Resource | Category | Function & Relevance | Example/Note |
|---|---|---|---|
| Software with FOCE & Full FIM | Computational Tool | Performs robust optimal design calculation for NLMEMs, minimizing clustering. | PFIM, PopED, Pumas [8] [3]. |
| FSP Solver Software | Computational Tool | Solves the Chemical Master Equation for stochastic systems to enable FSP-FIM calculation. | MATLAB's FSP package, FiniteStateProjection.jl in Julia [55]. |
| Clinical Trial Simulation (CTS) Pipeline | Computational Method | Validates optimal designs by simulating and re-estimating many datasets to assess empirical performance [56] [8]. | Essential step before finalizing any design. |
| Adaptive Gaussian Quadrature (AGQ) Library | Computational Library | Enables accurate numerical integration for likelihoods in mixed-effects models [56]. | statmod package in R [56]. |
| Single-Molecule FISH (smFISH) Probes | Experimental Reagent | Generates the discrete, single-cell snapshot data for which FSP-FIM is designed [55]. | Provides absolute counts of mRNA transcripts. |
| Microfluidics / Optogenetics Setup | Experimental Platform | Enables precise temporal perturbations and controlled environments for model-driven optimal experiments [55]. | Used to implement stimuli at FIM-optimized time points. |
Diagram: The Gap Between Asymptotic Theory and Practical Experiment
Diagram: The conceptual gap between asymptotic FIM theory and practical experimental constraints.
This technical support center provides targeted troubleshooting and guidance for researchers integrating Monte Carlo simulation with Fisher information matrix-based optimal experimental design. This approach is central to developing robust, efficient, and fair clinical prediction models and pharmacometric analyses in drug development [57] [58] [14]. The following sections address common computational, statistical, and design challenges, offering step-by-step solutions and best practices.
Troubleshooting Guide
Section 1: Monte Carlo Simulation Challenges
Monte Carlo simulations are used to model uncertainty, but their implementation can present specific issues [57] [59].
Problem 1: Inefficient Sampling Leading to Prolonged Run Times
- Symptoms: A single model evaluation takes an excessively long time; achieving stable results requires an impractical number of iterations (e.g., >100,000) [57].
- Diagnosis: This is often caused by naive random sampling of high-dimensional parameter spaces or complex, computationally expensive model functions.
- Solution:
- Profile your code to identify the most computationally intensive functions.
- Implement variance reduction techniques such as Latin Hypercube Sampling or importance sampling to improve efficiency.
- Consider parallelization. Most Monte Carlo simulations are "embarrassingly parallel." Use parallel computing frameworks (e.g., R's
parallel, Python'smultiprocessing) to distribute iterations across multiple CPU cores. - For a fixed computational budget, prioritize increasing the number of iterations over model complexity to reduce the standard error of your estimates [57].
Problem 2: Unrealistic or Overly Narrow Outcome Distributions
- Symptoms: Simulation results show an unrealistically small range of outcomes; the model fails to reproduce the tail risks observed in real-world data.
- Diagnosis: The input probability distributions for key uncertain parameters (e.g., clinical trial failure rates, cost overruns) are incorrectly specified, often using single-point estimates instead of ranges [59].
- Solution:
- Replace point estimates with quantified uncertainty. For each critical input, define a range (e.g., a 90% confidence interval) based on historical data or expert elicitation [59].
- Choose appropriate distributions. Use log-normal distributions for strictly positive costs, beta distributions for probabilities, and multivariate distributions to capture parameter correlations.
- Validate and calibrate your input distributions against any available pilot study or historical cohort data [58].
Problem 3: Handling Dependencies Between Projects in Portfolio Analysis
- Symptoms: The simulated value of a drug development portfolio does not correctly reflect the impact of a lead compound's success or failure on follower projects.
- Diagnosis: The models for individual projects are run in isolation, ignoring strategic dependencies [59].
- Solution:
- Map the dependency network. Clearly define how the outcome of one project (e.g., successful Phase III trial) gates or influences the parameters of others (e.g., initiation, budget allocation) [59].
- Build conditional logic into the simulation framework. Program your model so that the random outcome of a "parent" project dynamically adjusts the inputs or triggers the start of "dependent" projects within the same simulation run.
- Analyze the results to identify which dependencies create the greatest sources of portfolio value or risk concentration.
Section 2: Fisher Information Matrix & Optimal Design Challenges
Optimal design using the Fisher Information Matrix (FIM) is key to precise parameter estimation, but its application can be complex [58] [14] [60].
Problem 1: High Uncertainty in Individual-Level Predictions Despite Adequate Sample Size
- Symptoms: A developed clinical prediction model has good overall calibration but produces implausibly wide confidence intervals for individual risk estimates, making it unsuitable for clinical decision-making [58].
- Diagnosis: The study sample size was calculated only for population-level criteria (e.g., overall risk estimation, minimizing overfitting) and is insufficient for precise individual-level predictions [58].
- Solution:
- Use the FIM decomposition method. Employ the five-step process outlined by Ensor et al. (2025) [58] to calculate the variance of an individual's risk estimate before data collection.
- Specify a core set of predictors and their joint distribution. This is required to compute the unit information matrix [58].
- Utilize software tools like the
pmstabilityssmodule in Stata or R to calculate the sample size needed to achieve a pre-specified width for the uncertainty interval of individual predictions [58].
Problem 2: Selecting an Appropriate Optimality Criterion for Design
- Symptoms: Uncertainty about which statistical criterion (e.g., D-, A-, G-optimality) to use when optimizing an experimental design for a pharmacometric study [60].
- Diagnosis: The choice of optimality criterion depends on the primary goal of the experiment (precise parameter estimates vs. precise predictions) [60].
- Solution: Refer to the following table to match your experimental goal with the correct criterion:
| Optimality Criterion | Primary Goal | Common Application in Pharmacometrics |
|---|---|---|
| D-Optimality | Maximize the overall precision of all parameter estimates (minimize the joint confidence region). | Optimizing sampling schedules for population PK/PD model estimation [14] [60]. |
| A-Optimality | Minimize the average variance of the parameter estimates. | Useful when the focus is on a set of parameters with similar importance [60]. |
| C-Optimality | Minimize the variance of a specific linear combination of parameters (e.g., AUC). | Optimizing design to estimate a specific derived parameter of interest [60]. |
| G- or V-Optimality | Minimize the maximum or average prediction variance over a region of interest. | Designing experiments where accurate prediction of the response is the key objective [60]. |
- Problem 3: Incorporating Discrete and Continuous Covariates in FIM Calculation
- Symptoms: Difficulty computing the expected FIM for a population design when the model includes both continuous (e.g., weight, age) and discrete (e.g., sex, genotype) covariates [14].
- Diagnosis: The standard FIM calculation may not adequately account for the joint distribution of mixed covariate types.
- Solution:
- Use the extended FIM method. As implemented in tools like the R package
PFIM, the FIM's expectation can be computed over the joint covariate distribution [14]. - Provide a sample of covariate vectors from an existing dataset or pilot study.
- Simulate covariate vectors based on provided marginal distributions, or use copula-based methods to model their dependencies [14].
- This approach allows for accurate prediction of uncertainty on covariate effects and the power to detect clinically relevant relationships [14].
- Use the extended FIM method. As implemented in tools like the R package
Frequently Asked Questions (FAQs)
Q1: What is the fundamental advantage of using Monte Carlo simulation over deterministic modeling in drug development? A: Monte Carlo simulation explicitly accounts for uncertainty and variability in inputs (e.g., trial success probability, patient recruitment rate). Instead of producing a single, often misleading, point estimate, it generates a probability distribution of possible outcomes, allowing for risk-adjusted decision-making and the identification of "what you don't know you don't know" [59].
Q2: How does the Fisher Information Matrix relate to the precision of a prediction model? A: The Fisher Information Matrix (FIM) quantifies the amount of information a sample of data carries about the model's unknown parameters. The inverse of the FIM provides an estimate of the variance-covariance matrix for the parameters [60]. Therefore, maximizing the FIM (through optimal design) directly minimizes the variance of parameter estimates, leading to more precise and stable model predictions [58] [60].
Q3: My sample size meets the "events per variable" rule of thumb. Why is my model still unstable for individual predictions? A: Traditional rules of thumb target parameter estimation but often ignore the case-mix distribution [58]. For precise individual-level predictions, the sample must adequately represent all relevant combinations of predictor values (covariate strata). A decomposition of the FIM can reveal if your sample size provides sufficient information for reliable predictions across the entire target population [58].
Q4: When should I use a sequential or adaptive experimental design? A: Sequential designs are powerful when experiments are run in stages and early results can inform later stages. They are particularly valuable in early-phase clinical trials or when resource constraints are severe. Adaptive designs use pre-planned rules to modify the trial based on interim data (e.g., re-estimating sample size), offering greater efficiency but increased operational complexity [60].
Q5: What are common software tools for implementing these methods? A: Several specialized tools exist:
- Monte Carlo Simulation: General-purpose: @RISK (Excel),
mc2d(R). Drug development: Captario SUM, Pharmap. - Optimal Design & FIM:
PFIM(R) for pharmacometrics [14],PopED,pmsampsizeandpmstabilityss(Stata/R) for prediction model sample size [58]. - General Optimization & DOE: JMP, SAS
proc optex, R packagesAlgDesign,DiceDesign.
Experimental Protocols & Methodologies
This protocol uses a decomposition of the Fisher Information Matrix to determine the sample size needed for stable individual-level predictions from a binary outcome model.
1. Identify Core Predictors:
- Select variables known to provide essential predictive information, based on prior models, literature, or clinical expertise [58].
- Include key demographic variables (e.g., age, sex, ethnicity) to enable fairness checks across subgroups [58].
2. Specify Joint Predictor Distribution:
- If an existing dataset is available: Use the observed joint distribution directly.
- If planning a new study: Specify the anticipated distribution. Use published statistics, pilot data, or generate a synthetic dataset reflecting the target population case-mix [58].
3. Define the Anticipated Core Model:
- Specify the logistic regression equation, including assumed coefficients for the core predictors.
- Alternatively, specify the model's anticipated overall discrimination (C-statistic) and the relative effect sizes of standardized predictors [58].
4. Calculate Unit Information & Variance:
- The variance of the linear predictor for an individual i is decomposed as:
Var(η_i) = x_i' * (n * M)^-1 * x_i, wherex_iis the individual's predictor vector,nis the total sample size, andMis the unit Fisher information matrix (the expected information per observation) [58]. - Software like
pmstabilityssautomates this calculation.
5. Determine Sample Size for Target Precision:
- Specify a target maximum acceptable width for the confidence interval of an individual's predicted risk.
- Iteratively calculate the required sample size
nneeded to achieve this precision across a representative set of covariate patterns, particularly for critical subgroups [58].
This protocol is used in pharmacometrics to assess the power to detect significant covariate relationships in a Non-Linear Mixed Effects Model (NLMEM).
1. Define the Base Population PK/PD Model:
- Start with a previously developed model, including fixed effects, random effects, and residual error model.
- Identify the parameters for which covariate relationships will be tested (e.g., effect of renal function on clearance).
2. Specify Covariate Models and Distributions:
- Define the mathematical form of the covariate relationship (e.g., linear, power).
- Specify the distributions (continuous/discrete) for all covariates in the target population. Use historical data or simulate from marginal distributions and copulas [14].
3. Compute the Expected FIM:
- Using software (e.g.,
PFIM), compute the expected FIM for a proposed design (sample size, sampling times). - The calculation integrates over the specified joint distribution of covariates [14].
4. Derive Uncertainty and Power:
- From the inverse of the FIM, obtain the predicted variance for each covariate parameter estimate.
- For Significance Testing: Calculate the power of the Wald test to reject the null hypothesis (covariate effect = 0).
- For Relevance Testing: Calculate the power of a Two One-Sided Test (TOST) procedure to conclude that the covariate effect lies within a pre-defined interval of clinical irrelevance (analogous to bioequivalence testing) [14].
5. Optimize Design and Iterate:
- Adjust the design (e.g., increase sample size, change sampling schedule) and repeat steps 3-4 until the predicted power for key covariate relationships meets the desired threshold (e.g., 80%).
Visualizations: Workflows and Relationships
Diagram 1: Integrated Workflow for Simulation-Informed Optimal Design
This diagram illustrates the iterative cycle of using Monte Carlo simulation and Fisher Information to optimize experiments and validate models.
Integrated Workflow for Simulation-Informed Optimal Design
Diagram 2: Decision Logic for Selecting an Optimality Criterion
This flowchart guides the researcher in selecting the most appropriate optimality criterion based on their primary experimental objective [60].
Decision Logic for Selecting an Optimality Criterion
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential computational and methodological "reagents" for implementing the discussed frameworks.
| Item/Category | Function & Purpose | Key Examples & Notes |
|---|---|---|
| Optimality Criteria (Theoretical) | Mathematical objectives used to evaluate and optimize an experimental design based on the Fisher Information Matrix (FIM) [60]. | D-optimality: Maximizes determinant of FIM. Best for precise parameter estimation [60]. G-optimality: Minimizes maximum prediction variance. Best for response surface accuracy [60]. |
| Variance Reduction Techniques | Algorithms to increase the statistical efficiency of Monte Carlo simulations, reducing the number of runs needed for a stable result. | Latin Hypercube Sampling: Ensures full stratification of input distributions. Importance Sampling: Oversamples from important regions of the input space. |
| Software for FIM & Design | Specialized tools to compute the FIM, optimize designs, and calculate related sample sizes and power. | PFIM (R): For optimal design in NLMEM [14]. pmsampsize/pmstabilityss: For prediction model sample size [58]. JMP, SAS proc optex: General DOE suites. |
| Synthetic Data Generators | Methods/packages to create plausible, privacy-preserving datasets that mimic the joint distribution of predictors for planning purposes. | synthpop (R package): Generates synthetic data with similar statistical properties to an original dataset [58]. Crucial for step 2 of the sample size protocol when primary data is unavailable. |
| Parallel Computing Framework | Infrastructure to execute thousands of independent Monte Carlo simulation runs simultaneously, drastically reducing computation time. | R: parallel, future, foreach. Python: multiprocessing, joblib, dask. Essential for complex models or large-scale portfolio simulations [59]. |
Troubleshooting Guide: Common Experimental Design & Analysis Issues
This guide addresses specific challenges you may encounter when designing experiments and analyzing data within the framework of optimal design and information matrix theory.
Problem 1: Low Precision in Key Parameter Estimates
- Symptoms: Wide confidence intervals for model parameters; high standard errors in parameter estimation; sensitivity analysis shows estimates are unstable.
- Diagnosis: The experimental design provides insufficient Fisher Information for the parameters of interest. The Fisher Information Matrix (FIM) quantifies the amount of information your data carries about the parameters [3]. A small FIM determinant (D-criterion) indicates a suboptimal design.
- Solution:
- Calculate the FIM: For your model and proposed design
d, compute the expected FIM,I(θ; d). Its diagonal elementsI_iirepresent the information about parameterθ_i[3]. - Apply Optimality Criteria: Optimize your design
dby maximizing a scalar function ofI(θ; d). For overall precision, maximize the D-criterion (determinant of FIM). To minimize the variance of a specific parameter, maximize the A-criterion (trace of the inverse FIM) [3]. - Implement Design Augmentation: Use sequential design strategies. Collect initial data, estimate parameters, and then calculate an optimal design for the next experimental run based on the updated parameter estimates.
- Calculate the FIM: For your model and proposed design
Problem 2: Biased Sampling (e.g., Length-Bias) in Observational Studies
- Symptoms: Survival or duration estimates are systematically skewed (e.g., longer than expected); sample is not representative of the incident population.
- Diagnosis: Prevalent cohort sampling, where subjects are selected based on having experienced an initiating event (e.g., disease diagnosis), leads to length-biased sampling. Individuals with longer durations are over-represented [61].
- Solution:
- Identify the Bias: Confirm if your data collection follows a prevalent sampling scheme rather than an incident (random) sampling scheme.
- Use Bias-Adjusted Methods: Do not use the standard Kaplan-Meier estimator. Employ methods specifically developed for length-biased, right-censored data, such as the nonparametric maximum likelihood estimator (NPMLE) [61].
- Construct Valid Confidence Intervals: Use the empirical likelihood (EL) method to construct confidence intervals for the mean, median, or survival function. The EL ratio method can be adapted for right-censored length-biased data without requiring complex variance estimation [61].
Problem 3: Poor Coverage of Confidence Intervals for Standardized Effect Sizes
- Symptoms: For small sample studies, the empirically observed coverage of your 95% confidence intervals (CIs) is consistently below 95%.
- Diagnosis: Using simple approximate methods or the wrong parameterization for small-sample CI construction for standardized mean differences (e.g., Cohen's d). The sample standardized mean difference
dis a biased estimator of the population effectδ[62]. - Solution:
- Choose the Correct Method: For small sample sizes (
n< 20 per group), avoid the Hedges & Olkin method with the biasedd(Hd), which can have coverage as low as 86% [62]. - Recommended Method: Use the Steiger & Fouladi method with the biased estimator
d(Sd). Simulations show it produces confidence intervals closest to the nominal 95% coverage across various effect sizes and sample sizes [62]. - Alternative: Use the Hedges & Olkin method with the unbiased estimator
g(Hg). While coverage dips slightly (93-94%) for very small samples (n=5-15), it is consistent across effect sizes [62].
- Choose the Correct Method: For small sample sizes (
Table: Troubleshooting Summary for Confidence Interval Coverage
| Problem | Sample Size Context | Recommended Method | Key Reason |
|---|---|---|---|
| Poor CI coverage for standardized mean difference | Small samples (n < 40/group) | Steiger & Fouladi (Sd) [62] | Maintains coverage nearest to 95% for all n > 5. |
| Poor CI coverage for standardized mean difference | Small samples, unbiased focus | Hedges & Olkin (Hg) [62] | Uses unbiased g; consistent coverage across effect sizes. |
| CI for mean/quantile with length-biased data | Prevalent cohort studies | Empirical Likelihood (EL) [61] | Adapts to biased sampling without complex variance formulas. |
Problem 4: High Empirical Covariance Between Parameter Estimates
- Symptoms: Strong correlation in the variance-covariance matrix of parameter estimates; difficulty in isolating the effect of one parameter.
- Diagnosis: The off-diagonal elements of the Fisher Information Matrix (
I_ijwherei ≠ j) are large, indicating that the data does not inform the parameters independently [3]. The design does not allow the parameters to be precisely estimated simultaneously. - Solution:
- Re-parameterize the Model: If possible, reformulate the model to reduce parameter dependence.
- Re-optimize the Design: Use the V-criterion or modified E-criterion, which are specifically aimed at minimizing the variance (or maximum variance) of predicted parameters or functions of parameters. This directly addresses the covariance structure.
- Stagger Experiments: Design a sequence of experiments where early runs are optimized to reduce covariance for a subset of parameters, informing later, more precise designs.
Frequently Asked Questions (FAQs)
Q1: What is the practical relationship between the Fisher Information Matrix (FIM) and the confidence intervals I calculate from my data? A1: The FIM is a pre-experiment predictive tool. Its inverse provides the Cramér-Rao lower bound—the minimum possible variance for an unbiased parameter estimator given your proposed design [3]. While the actual confidence intervals from your data will be based on the observed information (or covariance matrix), a design that maximizes the FIM (e.g., D-optimal design) minimizes this lower bound, giving you the best possible chance of obtaining tight, precise confidence intervals from the eventual experiment.
Q2: When should I be concerned about bias in my effect size estimate, and how does it impact interval estimation? A2: Bias is a critical concern with small samples or non-random sampling. For example, the common standardized mean difference (d) is biased upward, especially with degrees of freedom below 20 [62]. This bias distorts the center of the confidence interval. You can either:
- Construct the interval around the biased estimate using a method that accounts for its sampling distribution (e.g., the Sd method) [62].
- Use an unbiased estimator like g and construct the interval around it (e.g., the Hg method) [62]. The choice influences coverage properties, as outlined in the troubleshooting guide.
Q3: What is the core difference between "empirical covariance" from data and the covariance predicted by the FIM? A3: Empirical covariance is calculated after the experiment from your actual data set, reflecting the observed joint variability of your parameter estimates. It is the "realized" covariance. The covariance predicted by the inverse FIM is an a priori expectation based on your statistical model and proposed experimental design. A well-designed experiment will show close alignment between the predicted and empirical covariance. A large discrepancy may indicate model misspecification or problems with the experimental execution.
Q4: How do I validate that my D-optimal design performed as expected? A4: Performance validation requires simulation:
- Fix your model parameters at a plausible value.
- Simulate hundreds or thousands of synthetic data sets using your D-optimal design protocol.
- Analyze each simulated data set to estimate parameters and compute confidence intervals.
- Calculate empirical coverage probabilities (the proportion of intervals containing the true parameter) and the average empirical standard errors. Compare these empirical results to the predictions from the FIM (e.g., the square root of the diagonal of the inverse FIM gives predicted standard errors) [3]. This simulation-based validation is considered best practice before committing to a costly experiment.
Experimental Protocols
Protocol 1: Constructing Empirical Likelihood Confidence Intervals for Length-Biased Data
Application: Estimating confidence intervals for the mean, median, or survival function from right-censored, length-biased data (e.g., prevalent cohort studies) [61]. Steps:
- Data Preparation: For each subject
i, record the observed timeX_i(from onset to failure or censoring) and the censoring indicatorδ_i(1 for failure, 0 for censored). - Specify Estimating Equation: For the target parameter
η(e.g., meanμ), define an unbiased estimating equation under the length-biased model. For the mean, this isΣ_i w_i * (X_i - μ) = 0, where weightsw_iare derived from the NPMLE of the biased distributionG. - Maximize Empirical Likelihood: Compute the empirical likelihood ratio statistic
R(η)by maximizing the nonparametric likelihood subject to the constraint imposed by the estimating equation. - Calibrate with Chi-Square: Use the fact that
-2 log R(η0)asymptotically follows a chi-square distribution to find the values ofηthat form the(1-α)%confidence interval.
Protocol 2: Computing and Comparing Confidence Intervals for Standardized Mean Difference
Application: Comparing two independent groups (e.g., control vs. treatment) and constructing a confidence interval for Cohen's d or Hedges' g [62]. Steps:
- Calculate Effect Size:
- Select and Apply Method:
- For the Sd (Steiger & Fouladi) method:
a. Treat
d * sqrt(N)as a noncentraltvariate withνdf and noncentrality parameterλ = δ * sqrt(N). b. Find the value ofδfor which the observedtis at the 2.5th and 97.5th percentile of the noncentralt(ν, λ)distribution. Theseδvalues are the confidence limits ford. - For the Hg (Hedges & Olkin) method:
a. Repeat the Sd method process, but using
ginstead ofdas the starting point. b. The resulting confidence interval will be for the unbiased population effect size.
- For the Sd (Steiger & Fouladi) method:
a. Treat
Visual Workflows and Relationships
Diagram 1: From Design Factors to Optimal Design (96 characters)
Diagram 2: D-Optimal Design Iterative Workflow (88 characters)
Table: Key Resources for Optimal Design & Analysis Research
| Resource Name | Type | Primary Function in Research | Example/Tool |
|---|---|---|---|
| Fisher Information Matrix Calculator | Software Module | Computes the expected FIM for a given nonlinear model and experimental design protocol. Essential for pre-experiment design optimization. | PopED (R), PFIM (standalone), Pumas [3], MONOLIX |
| Noncentral t-Distribution Library | Statistical Library | Enables exact calculation of confidence intervals for standardized effect sizes (Cohen's d, Hedges' g) using methods like Steiger & Fouladi [62]. | MBESS R package, stats::pt (noncentral) in R, scipy.stats.nct in Python |
| Empirical Likelihood Package | Statistical Library | Provides functions to construct nonparametric confidence intervals for complex data structures, such as length-biased or censored data, without relying on variance estimators [61]. | emplik R package, EL package |
| Optimal Design Optimizer | Software Solver | Executes numerical optimization algorithms (e.g., exchange, simplex, stochastic) to find the design variables (times, doses) that maximize a chosen optimality criterion of the FIM. | Built-in optimizers in PopED, Pumas [3], MATLAB's fmincon, general-purpose optimizers in R/Python. |
| Statistical Simulation Framework | Programming Environment | Allows for Monte Carlo simulation to validate design performance, assess bias, and compute empirical coverage probabilities of confidence intervals. Critical for proof-of-design [3]. | R, Python with NumPy/SciPy, Julia, specialized simulation languages. |
| Bias Correction Function | Computational Formula | Implements the correction factor J(ν) to convert the biased standardized mean difference d to the unbiased estimator g [62]. | Self-coded in analysis script, available in effectsize R package. |
Welcome to the Technical Support Center for Optimal Experimental Design (OED). This resource is dedicated to supporting researchers, scientists, and drug development professionals in implementing robust OED strategies, with a specialized focus on methodologies involving the Fisher Information Matrix (FIM). The FIM is a fundamental statistical tool that quantifies the amount of information data carries about model parameters, and its maximization is key to minimizing parameter uncertainty in experiments [30] [2]. This guide synthesizes findings from comparative literature to provide practical troubleshooting, protocols, and resources for your research.
Troubleshooting Guides: Common FIM Implementation Challenges
This section addresses frequent issues encountered when designing experiments using FIM-based optimal design, drawing on comparative case studies [8] [11].
Design Optimization Issues
Problem: My D-optimal sampling design yields heavily clustered sampling times, which seems suboptimal for model robustness.
- Cause: This is a known outcome when using the First Order (FO) approximation with a block-diagonal FIM implementation for models where the number of samples per individual exceeds the number of parameters. This combination can artificially reduce the number of unique "support points" in the design [8].
- Solution & Reference: Switch to using a First Order Conditional Estimation (FOCE) approximation with a Full FIM implementation. Comparative studies show this combination consistently produces designs with more support points and less clustering, which enhances robustness against model parameter misspecification [8].
- Preventive Measure: Prior to finalizing a design, compare the support point structure from different FIM approximation (FO vs. FOCE) and implementation (Full vs. Block-Diagonal) combinations. Validate the chosen design via simulation (see Protocol 1 below).
Problem: My optimal design performs well in theory (high FIM determinant) but yields biased parameter estimates when simulated data is analyzed.
- Cause: The FO approximation, particularly when paired with a block-diagonal FIM, can lead to designs with higher parameter bias, especially under model misspecification. The approximation may fail to capture true uncertainty structures [8].
- Solution & Reference: Use the FOCE approximation for design optimization, as it provides a more accurate linearization of the model around conditional estimates of random effects. Empirical evaluations show FOCE-based designs result in lower bias [8].
- Preventive Measure: Always evaluate the design performance through stochastic simulation and estimation (SSE), which provides an empirical covariance matrix, rather than relying solely on the theoretical FIM [8].
Problem: The numerical optimization for my model-based design of experiments (MBDoE) is computationally intensive, prone to local optima, and struggles with parametric uncertainty.
- Cause: Traditional MBDoE relies on solving a potentially non-convex optimization problem, which is computationally costly and sensitive to initial guesses and parameter uncertainty [11].
- Solution & Reference: Consider an optimization-free Fisher Information Matrix Driven (FIMD) approach. This method iteratively selects the most informative experiment from a candidate set based on FIM ranking, bypassing the traditional optimization loop and achieving faster convergence with less computational burden [11].
- Preventive Measure: For online or adaptive experimental design where speed is critical, implement the FIMD algorithm. It is particularly effective for kinetic model identification in chemical processes [11].
Computational & Practical Challenges
Problem: Computing the full FIM for my complex nonlinear mixed-effects model (NLMEM) is prohibitively slow.
- Cause: The full FIM calculation has high numerical complexity. For initial scoping or large models, this can be a bottleneck [8] [3].
- Solution & Reference: Employ the block-diagonal FIM approximation, which assumes independence between fixed effects and variance parameters, to speed up calculations. For final design validation, the full FIM or SSE is recommended. In machine learning contexts, diagonal FIM approximations are used to manage high-dimensional parameter spaces [8] [30].
- Preventive Measure: Use a tiered approach: perform initial design screening with a block-diagonal FIM, then refine and validate the top candidates using the full FIM or SSE.
Problem: I need to compute the FIM for a model where the likelihood is intractable or for a non-parametric scenario.
- Cause: The classical FIM definition requires derivatives of the log-likelihood, which may not be available [30].
- Solution & Reference: Utilize simulation-based estimators. Monte Carlo methods can estimate the FIM by averaging score functions or Hessians over simulated data. For non-parametric cases, methods like f-divergence expansions or the Pearson Information Matrix (a lower bound based on moments) can be applied [30].
- Preventive Measure: Leverage modern automatic differentiation (autodiff) tools within software frameworks (e.g.,
Jax). Autodiff can compute exact Hessians or gradients for complex models, enabling accurate FIM calculation where analytical derivation is impossible [63].
The table below summarizes the performance and computational trade-offs of different FIM approximation strategies based on comparative studies:
Table 1: Comparative Performance of FIM Approximation Methods
| Approximation Method | Support Points & Clustering | Bias Under Misspecification | Computational Speed | Recommended Use Case |
|---|---|---|---|---|
| FO + Block-Diag FIM [8] | Fewer points, high clustering | Higher | Fastest | Initial screening, very large models |
| FO + Full FIM [8] | Intermediate | Lower than FO Block-Diag | Moderate | Standard design when FOCE is too slow |
| FOCE + Full FIM [8] | More points, less clustering | Lowest | Slowest (per iteration) | Final robust design for complex NLME models |
| Optimization-Free (FIMD) [11] | Depends on candidate set | Comparable/Good | Fast convergence | Online/adaptive design, avoiding optimization |
Detailed Experimental Protocols
Protocol 1: Comparative Evaluation of FIM-Based Designs via Simulation
This protocol is derived from the methodology used to compare FO and FOCE approximations [8].
- Model & Design Definition: Define your NLME model (structural, inter-individual variability, residual error) and the design variables to optimize (e.g., sampling times).
- Generate Optimal Designs: Compute D-optimal designs using different target FIM configurations (e.g., FO/Block-diagonal, FO/Full, FOCE/Full). Use optimal design software (e.g., PopED, PFIM).
- Stochastic Simulation & Estimation (SSE):
a. Simulate
N(e.g., 500-1000) datasets for each optimal design, using the true model parameters. b. Estimate parameters from each simulated dataset using a pre-specified estimation method (e.g., FOCE with interaction). c. Calculate the empirical covariance matrix (empCOV) from theNsets of parameter estimates. d. Compute the empirical D-criterion asdet(empCOV^(-1)). Generate a confidence interval for this criterion using bootstrap methods. - Evaluate Robustness: a. Repeat Step 3, but simulate data using a set of misspecified parameter values (different from those used in Step 2 for optimization). b. Compare the empirical D-criteria and parameter bias across the different designs. The design that maintains the highest D-criterion (smallest parameter uncertainty) and lowest bias under misspecification is the most robust.
Protocol 2: Implementing an Optimization-Free FIMD Approach
This protocol outlines the core workflow of the Fisher Information Matrix Driven method [11].
- Candidate Experiment Generation: Define the operational space of your experiment (e.g., range of temperatures, concentrations, time points). Generate a large, diverse set of candidate experimental conditions.
- Initialization: Start with an initial dataset (from prior experiments or a small set of seed points).
- Iterative Loop: a. Ranking: For each candidate experiment, compute the predicted FIM (or a scalar optimality criterion like D-optimality) conditional on the current data and the candidate. This evaluates the expected information gain. b. Selection: Select the candidate experiment with the highest ranking (i.e., the one that maximizes the expected information). c. Execution & Update: Perform the selected physical experiment, obtain the new data, and update the model parameter estimates (e.g., via maximum likelihood). d. Convergence Check: Repeat steps a-c until a stopping criterion is met (e.g., parameter uncertainty falls below a threshold, or a maximum number of runs is reached).
Workflow Visualizations
FIM Approximation Comparison Workflow
Optimization-Free FIMD Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Reagents and Tools for FIM-Based Optimal Design Studies
| Item / Solution | Function in Optimal Design Research | Example from Literature |
|---|---|---|
| Nonlinear Mixed-Effects Modeling Software | Platform for implementing PK/PD models, calculating FIM approximations, and performing design optimization. Essential for executing Protocols 1 & 2. | Used with PopED, PFIM, Pumas for Warfarin PK design [8] [3]. |
| Monte Carlo Simulation Engine | Tool for stochastic simulation and estimation (SSE) to empirically evaluate and validate design performance beyond theoretical FIM. | Used to compute empirical D-criterion confidence intervals [8]. |
| Automatic Differentiation Framework | Library (e.g., Jax, Stan) that enables efficient and accurate computation of gradients and Hessians for complex models, facilitating FIM calculation. | Used for computing the Hessian of the loss function in optical system design [63]. |
| Standard Pharmacokinetic Model Compound | Well-characterized reference drug for developing and testing optimal design methodologies in a known system. | Warfarin PK model used as a standard example [8]. |
| Bench-scale Bioreactor System | Platform for implementing and validating optimal experimental designs in dynamic, resource-intensive processes like fermentation. | Fed-batch baker's yeast fermentation case study [11]. |
| Flow Chemistry Reactor System | Platform for testing online, adaptive optimal design strategies for chemical reaction kinetics. | Nucleophilic aromatic substitution case study [11]. |
Frequently Asked Questions (FAQs)
Q: What is the practical implication of the Cramér-Rao Lower Bound in my experiment? A: The inverse of the FIM provides a lower bound for the variance of any unbiased parameter estimator [2]. Maximizing the FIM (e.g., through D-optimal design) minimizes this lower bound, meaning you are designing an experiment with the theoretically smallest possible parameter uncertainty. In practice, it's a powerful surrogate objective for achieving precise estimates [3].
Q: When should I use the Full FIM versus the Block-Diagonal FIM? A: Use the block-diagonal FIM for faster computation during initial design scoping or for very large models, acknowledging it may produce clustered designs [8]. Use the full FIM for final design optimization and validation, as it accounts for correlations between fixed and random effect parameters and generally leads to more robust designs, especially when paired with FOCE [8].
Q: Is the traditional optimization-based MBDoE or the new optimization-free FIMD approach better for my project? A: It depends on the context. Traditional MBDoE is well-established for offline design where computational time is less critical and a global optimum is sought. The optimization-free FIMD approach is advantageous for online/adaptive design where experiments are run sequentially, when computational speed is paramount, or when the optimization landscape is complex and prone to local minima [11].
Q: How do I handle FIM calculation for a non-Gaussian or highly nonlinear model? A: For moderately non-Gaussian models, higher-order approximations like FOCE are crucial [8]. For severely non-Gaussian likelihoods (e.g., in gravitational-wave analysis), consider methods like the Derivative Approximation for Likelihoods (DALI) that use higher-order derivatives of the likelihood for more accurate approximations [30]. Simulation-based FIM estimation using Monte Carlo methods is another robust, general-purpose alternative [30].
Conclusion
The Fisher Information Matrix stands as a cornerstone for achieving precision and efficiency in biomedical experimental design. As demonstrated, a deep understanding of its foundation—the Cramér-Rao bound—is essential for setting realistic goals[citation:4]. Methodologically, the field is advancing beyond traditional optimization, offering faster, ranking-based strategies suitable for online and autonomous experimentation platforms[citation:1]. However, these powerful tools require careful application; the choice of model linearization (FO/FOCE) and FIM implementation can significantly impact the robustness of a design, especially when pre-existing parameter knowledge is uncertain[citation:2]. Therefore, validation through simulation-based methods remains a non-negotiable step for confirming design performance before committing valuable resources to a clinical or laboratory study. Future directions point toward the broader integration of these OED principles into adaptive clinical trials, the development of AI-assisted design tools, and continued refinement of methods to handle complex, high-dimensional biological models. By mastering the FIM framework outlined here, researchers and drug developers can systematically reduce uncertainty, minimize costs, and accelerate the translation of scientific discoveries into effective therapies.
References
- 1. - GeeksforGeeks Fisher Information [https://www.geeksforgeeks.org/machine-learning/fisher-information/]
- 2. Fisher information [https://en.wikipedia.org/wiki/Fisher_information]
- 3. Introduction to Optimal Design [https://tutorials.pumas.ai/html/introduction/optimal_design.html]
- 4. Advanced Methods for Dose and Regimen Finding During ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5529745/]
- 5. A Multi-Objective Optimal Experimental Design Framework ... [https://www.sciencedirect.com/science/article/pii/S2095809919308537]
- 6. Cramér–Rao bound [https://en.wikipedia.org/wiki/Cram%C3%A9r%E2%80%93Rao_bound]
- 7. Cramér–Rao bound [https://grokipedia.com/page/Cram%C3%A9r%E2%80%93Rao_bound]
- 8. The effect of Fisher information matrix approximation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5110617/]
- 9. Cramer-Rao Bound [https://www.geeksforgeeks.org/data-science/cramer-rao-bound/]
- 10. Proof of the Cramér–Rao Lower Bound [https://gregorygundersen.com/blog/2019/11/27/proof-crlb/]
- 11. An optimization-free Fisher information driven approach for ... [https://www.sciencedirect.com/science/article/pii/S009813542400142X]
- 12. Development and implementation of the population Fisher ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260700001176]
- 13. The effect of using a robust optimality criterion in model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5514236/]
- 14. Using Fisher Information Matrix to predict uncertainty in ... [https://www.medrxiv.org/content/10.1101/2024.10.16.24314758v1]
- 15. Sequential model-based A- and V-optimal design of ... [https://www.sciencedirect.com/science/article/abs/pii/S009813541930417X]
- 16. Practical identifiability in the frame of nonlinear mixed effects ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-021-04373-4]
- 17. Optimal experiment design with applications to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11996619/]
- 18. Optimal Experimental Design for Parameter Estimation of ... [https://www.mdpi.com/2227-9717/5/3/49]
- 19. Optimal design of population pharmacokinetic ... [https://www.page-meeting.org/Abstracts/optimal-design-of-population-pharmacokinetic-pharmacodynamic-studies/]
- 20. AI‐NLME: A New Artificial Intelligence‐Driven Nonlinear ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405737/]
- 21. A review on model-based design of experiments for ... [https://www.sciencedirect.com/science/article/pii/S0009250925011686]
- 22. Self-optimisation and model-based design of experiments ... [https://www.beilstein-journals.org/bjoc/articles/13/18]
- 23. A decomposition of Fisher's information to inform sample ... [https://pubmed.ncbi.nlm.nih.gov/40624575/]
- 24. Model-based design of experiments and measurement ... [https://curate.nd.edu/articles/dataset/Model-based_design_of_experiments_and_measurement_optimization_frameworks_based_on_scalable_and_tractable_algorithms_and_software/25607808]
- 25. Using design of experiments to guide genetic optimization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981448/]
- 26. 16.1. Model-Based Design of Experiments [https://ndcbe.github.io/data-and-computing/notebooks/16/Reaction-MBDoE.html]
- 27. Efficient Optimization of Stimuli for Model-Based Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4574939/]
- 28. Bayesian Optimisation VS “Classical” Design of ... [https://kufuu.eu/bayesian-optimisation-vs-classical-design-of-experiments/]
- 29. An optimization-free Fisher information driven approach for ... [https://discovery.ucl.ac.uk/id/eprint/10192727/]
- 30. Fisher Information Matrix Insights [https://www.emergentmind.com/topics/fisher-information-matrices]
- 31. Methods and software tools for design evaluation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4294071/]
- 32. Support software and resources [https://www.page-meeting.org/about-us/support-software-and-resources/]
- 33. Guidelines for the Quality Control of Population ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3475847/]
- 34. PKPD In Drug Discovery: Guiding Decisions With Modeling [https://www.pharmaron.com/knowledge-center/dmpk-insights-15-pkpd-drug-discovery/]
- 35. Overcoming PK / PD Modeling Challenges [https://www.pharmtech.com/view/overcoming-pk-pd-modeling-challenges]
- 36. Diversity in Trials : Optimizing Drug Development & Data Use [https://www.allucent.com/resources/blog/diversity-clinical-trials-optimizing-drug-development-strategy]
- 37. Linearization Method and the Resulting Algorithms [https://onlinehelp.certara.com/phoenix/8.5/Phoenix_UserDocs/NLMEEngines/Linearization_Method_and_the_Resulting_Algorithms.htm]
- 38. FO engine [https://onlinehelp.certara.com/phoenix/8.3/topics/FO_engine.htm]
- 39. Comparing the performance of FOCE and different ... [https://link.springer.com/article/10.1007/s10928-016-9476-y]
- 40. A Fast Method for Testing Covariates in Population PK/PD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3160160/]
- 41. Use of a linearization approximation facilitating stochastic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3969514/]
- 42. Fisher information matrix for nonlinear mixed effects ... [https://pubmed.ncbi.nlm.nih.gov/19266541/]
- 43. The effect of Fisher information matrix approximation ... [https://pubmed.ncbi.nlm.nih.gov/27804003/]
- 44. Methods and software tools for design evaluation... [https://www.ovid.com/journals/bjcpha/fulltext/10.1111/bcp.12352~methods-and-software-tools-for-design-evaluation-in]
- 45. Robust optimal designs using a model misspecification term [https://link.springer.com/article/10.1007/s00184-023-00893-6]
- 46. Frequently Asked Questions on Drug Development and ... [https://www.fda.gov/drugs/cder-small-business-industry-assistance-sbia/small-business-assistance-frequently-asked-questions-drug-development-and-investigational-new-drug]
- 47. Misspecification-robust Sequential Neural Likelihood for ... [https://arxiv.org/html/2301.13368v2]
- 48. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 49. FAQ & Troubleshooting [https://dispendix.com/knowledge-center]
- 50. Troubleshooting & FAQs [https://www.cygnustechnologies.com/resources/guidelines?srsltid=AfmBOooM3mBfGSt4xYuPCOf2SYcBcD3M3kDRUkhsGjCAp_NDw458QjZ_]
- 51. Robust Bayesian Optimal Experimental Design under Model ... [https://www.imsi.institute/videos/robust-bayesian-optimal-experimental-design-under-model-misspecification/]
- 52. Improving Robustness to Model Misspecification in ... [https://openreview.net/forum?id=uyNJLdCvFG]
- 53. Optimal experimental design: from design point to ... [https://link.springer.com/article/10.1007/s00362-025-01725-7]
- 54. Clustering of small molecules: new perspectives and their ... [https://www.frontiersin.org/journals/natural-products/articles/10.3389/fntpr.2024.1367537/full]
- 55. The finite state projection based Fisher information matrix ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6355035/]
- 56. A new method for evaluation of the Fisher information ... [https://www.sciencedirect.com/science/article/abs/pii/S0167947316302389]
- 57. Method “Monte Carlo” in healthcare - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11230067/]
- 58. A decomposition of Fisher's information to inform sample ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12235806/]
- 59. The Perks of Using Monte Carlo Simulations in Drug ... [https://www.captario.com/post/the-perks-of-using-monte-carlo-simulations-in-drug-development]
- 60. Optimal experimental design [https://en.wikipedia.org/wiki/Optimal_experimental_design]
- 61. Empirical likelihood-based confidence intervals for length- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4034580/]
- 62. Expected and empirical coverages of different methods for ... [https://link.springer.com/article/10.3758/s13428-021-01550-4]
- 63. Fisher Information - dLux [https://louisdesdoigts.github.io/dLux/tutorials/examples/fisher_information/]